Chapter: Case Study in Obstetrics and Gynaecology: Early Pregnancy
Case Study Reports: Vomiting in Pregnancy
VOMITING IN PREGNANCY
History
A
28-year-old Asian woman is referred
by her general practitioner (GP) with persistent vomiting at 7 weeks’
gestation. She is in her
second pregnancy having
had a normal vagi- nal delivery 3 years ago.
She is now
vomiting up to 10 times in 24 h, and has
not man- aged to tolerate any food for 3 days.
She can only drink small
amounts of water.
She
saw her GP a week ago who prescribed prochlorperazine suppositories but these
only helped for a few days.
She feels very weak in herself and is unable
to care for her son now.
On
direct questioning she
has upper abdominal pain that is constant, sharp
and burning. She has not opened
her bowels for 5 days.
She is passing small amounts
of dark urine infrequently but there is no dysuria
or haematuria. There
has been no vaginal bleeding.
There is no other
medical or gynaecological history of note except that she suffered
per- sistent vomiting in her first
pregnancy requiring two
overnight admissions.
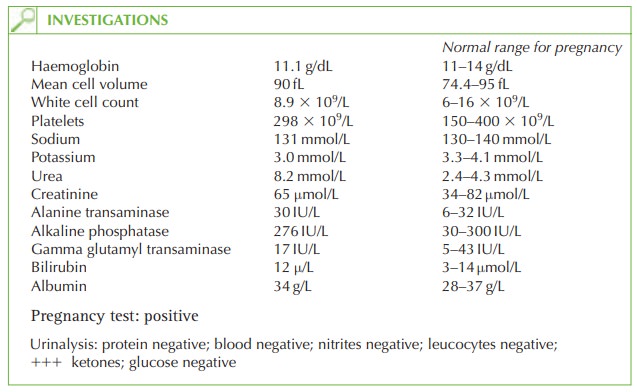
Examination
She is apyrexial. Lying blood
pressure is 115/68 mmHg and standing blood
pressure 98/55 mmHg. Heart
rate is 96/min.
The mucus membranes appear dry. Abdominal exam- ination reveals tenderness in the epigastrium but no lower
abdominal tenderness. The uterus is not palpable abdominally.
Questions
·
What is the diagnosis?
·
What are the potential
complications of this disorder?
·
How
would you further
investigate and manage this patient?
ANSWER
The
woman is suffering from hyperemesis gravidarum. This affects only less than 2 per cent
of pregnancies, although
more than 50 per cent of women
report some nausea
or vomiting when pregnant.
The
diagnosis in this case can be made because the urinalysis is negative apart
from the ketones, so urinary tract
infection is very unlikely. She has not opened her bowels but this
is likely to be secondary to poor dietary
intake and dehydration. Liver function is normal,
so liver disease causing vomiting
is unlikely (though
abnormal liver function
may occur as a result of hyperemesis itself). Thyroid function is normal, so an alternative diagnosis of hyperthyroidism causing
the vomiting is unlikely.
The
fetus is not at risk from hyperemesis and the nutritional deficiency in the mother does not
seem to affect
development. The risk
of miscarriage is lower in women with
hyper- emesis. The risk of twins
and molar pregnancy has traditionally been thought to be greater in women with hyperemesis, but this is refuted in more recent
research.
Further investigation and management
Hyperemesis is a self-limiting disease and the
aim of treatments is supportive, with discharge of the woman
once she is tolerating food and drink
and is no longer ketotic
on urinalysis.
·
Fluids:
3–4L of normal
saline should be infused per day. Dextrose solutions are contraindicated as they may precipitate Wernicke’s
encephaolopathy and also because the woman is hyponatraemic and needs normal saline.
·
Potassium: excessive vomiting generally
leads to hypokalaemia, and potassium chloride
should be administered with the normal saline according
to the serum electrolyte results.
·
Anti-emetics: first-line antiemetics include
cyclizine (antihistamine), metoclopramide (dopamine anatagonist) or
prochlorperazine (phenothiazine). In severe cases, ondansetron or domperidone may be effective. There is no evidence of teratogenicity
in humans from any of these regimes.
·
Thiamine and folic acid: vitamin B1 (thiamine) can prevent
Wernicke’s encephalopathy or the irreversible Korsakoff’s syndrome (amnesia, confabulation, impaired learning
ability).
·
Antacids: for epigastric pain
·
Total parenteral nutrition
(TPN):
TPN is rarely
indicated but may
be life saving
where all other management strategies have failed.
·
Thromboembolic stockings (TEDS) and heparin: women
with hyperemesis are at risk of
thrombosis from pregnancy, immobility and dehydration, and should be considered for low-molecular-weight heparin
regime as well as TEDS.
Monitoring
Daily monitoring should be carried
out, with weight measurement and urinalysis for ketones and renal and liver
function.
Related Topics