Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Thoracic Surgery
Anesthesia for Thoracic Surgery: The Lateral Decubitus Position
Physiological Considerations During Thoracic Anesthesia
Thoracic surgery presents a unique set
of physiologi-cal problems for the anesthesiologist. These include
physiological derangements caused by placing the patient in the lateral
decubitus position, opening the chest (open
pneumothorax), and the need for one-lung ventilation.
THE LATERAL DECUBITUS POSITION
The lateral decubitus position provides
optimal access for most operations on the lungs, pleura, esophagus, the great
vessels, other mediastinal structures, and vertebrae. Unfortunately, this
posi-tion may significantly alter the normal pulmonary ventilation/perfusion relationships. These
derange-ments are further accentuated by induction of anesthesia, initiation of
mechanical ventilation, neu-romuscular blockade, opening the chest, and
surgical retraction. Although perfusion continues to favor the dependent
(lower) lung, ventilation progressively favors the less perfused upper lung.
The resulting mismatch increases the risk of hypoxemia.
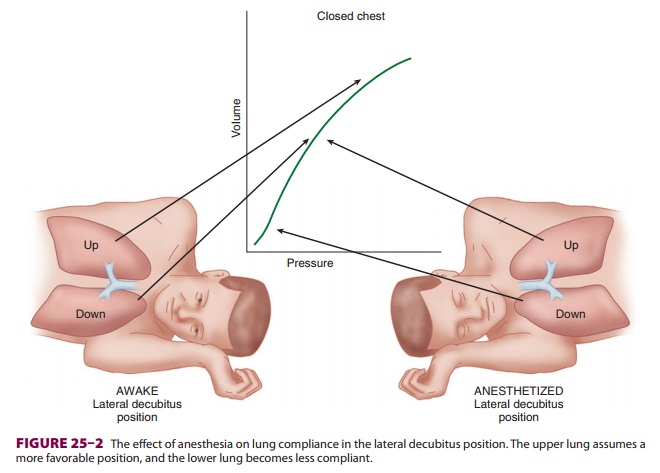
The Awake State
When a supine patient assumes the
lateral decu-bitus position, ventilation/perfusion matching is preserved during
spontaneous ventilation. The dependent (lower) lung receives more perfusion
than does the upper lung due to gravitational influ-ences on blood flow
distribution in the pulmonary circulation. The dependent lung also receives
more ventilation because: (1) contraction of the depen-dent hemidiaphragm is
more efficient compared with the nondependent [upper] hemidiaphragm and (2) the
dependent lung is on a more favorable part of the compliance curve ( Figure25–1).
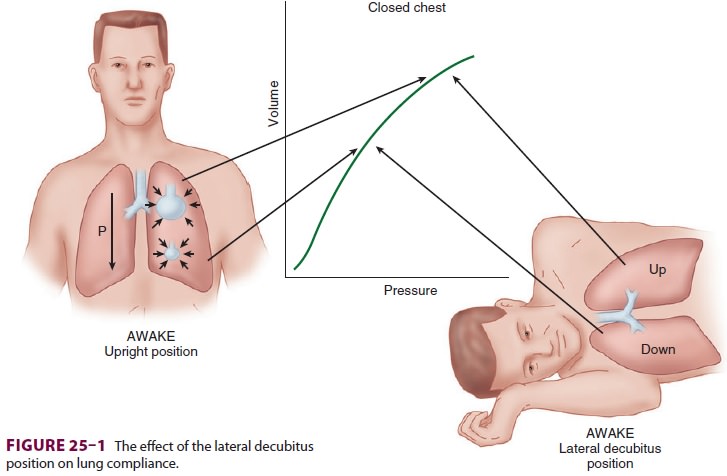
Induction of Anesthesia
The decrease in functional residual
capacity (FRC) with induction of general anesthesia moves the upper lung to a
more favorable part of the compliance
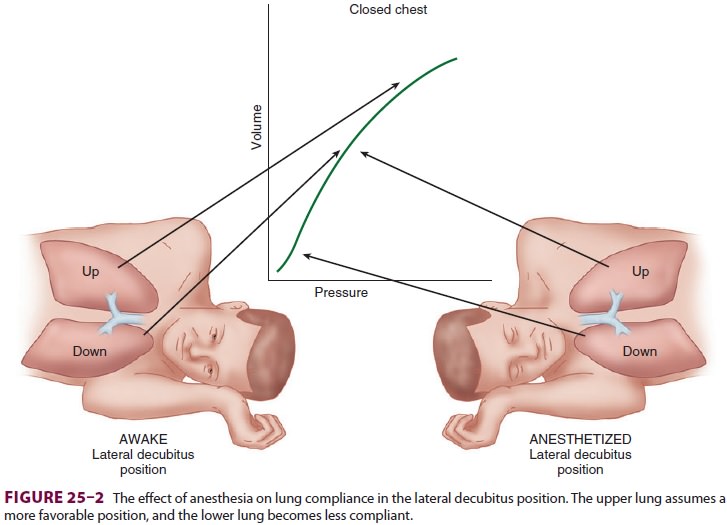
curve, but moves the lower lung to a
less favorable-position (Figure25–2). As a result, the upper lung is
ventilated more than the dependent lower lung; ven-tilation/perfusion mismatching occurs because the
dependent lung continues to have greater perfusion.
Positive-Pressure Ventilation
Controlled positive-pressure ventilation
favors the upper lung in the lateral position because it is more compliant than
the lower lung. Neuromuscular blockade enhances this effect by allowing the
abdominal contents to rise up further against the dependent hemidiaphragm and
impede ventila-tion of the lower lung. Using a rigid “bean bag” to maintain the
patient in the lateral decubitus position further restricts movement of the
dependent hemi-thorax. Finally, opening the nondependent side of the chest
further accentuates differences in compli-ance between the two sides because
the upper lung is now less restricted in movement. All of these effectsworsen
ventilation/perfusion
mismatching and pre-dispose the patient to hypoxemia.
Related Topics