Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Thoracic Surgery
Anesthesia for Lung Resection: Preoperative Considerations
Anesthesia for Lung Resection
PREOPERATIVE CONSIDERATIONS
Lung resections are usually carried out
for the diag-nosis and treatment of pulmonary tumors, and, less commonly, for
complications of necrotizing pulmo-nary infections and bronchiectasis.
1. Tumors
Pulmonary tumors can be either benign or
malig-nant, and, with the widespread use of bronchoscopic sampling, the
diagnosis is usually available prior to surgery. Hamartomas account for 90% of
benign pulmonary tumors; they are usually peripheral pul-monary lesions and
represent disorganized normal pulmonary tissue. Bronchial adenomas are usually
central pulmonary lesions that are typically benign, but occasionally may be
locally invasive and rarely metastasize. These tumors include pulmonary
car-cinoids, cylindromas, and mucoepidermoid adeno-mas. They often obstruct the
bronchial lumen and cause recurrent pneumonia distal to the obstruction in the
same area. Primary pulmonary carcinoids may secrete multiple hormones,
including adrenocortico-tropic hormone (ACTH) and arginine vasopressin;
however, manifestations of the carcinoid syndrome are uncommon and are more
likely with metastases.Malignant pulmonary tumors are divided into small
(“oat”) cell and non–small cell carcinomas.The latter group includes squamous
cell (epider-moid) tumors, adenocarcinomas, and large cell (anaplastic) carcinomas.
All types are more com-monly encountered in smokers, but more “never smokers”
die of lung cancer each year in the United States than the total number of
people who die of ovarian cancer. Epidermoid and small cell carcino-mas usually
present as central masses with bronchial lesions; adenocarcinoma and large cell
carcinomas are more typically peripheral lesions that often involve the pleura.
Clinical Manifestations
Symptoms may include cough, hemoptysis,
wheez-ing, weight loss, productive sputum, dyspnea, or fever. Pleuritic chest
pain or pleural effusion sug-gests pleural extension. Involvement of
mediastinal structures is suggested by hoarseness that results from compression
of the recurrent laryngeal nerve, Horner’s syndrome caused by involvement of
the sympathetic chain, an elevated hemidiaphragm caused by compression of the
phrenic nerve, dys-phagia caused by compression of the esophagus, or the
superior vena cava syndrome caused by compression or invasion of the superior
vena cava. Pericardial effusion or cardiomegaly suggests car-diac involvement.
Extension of apical (superior sulcus) tumors can result in either shoulder or
arm pain, or both, because of involvement of the C7–T2 roots of the brachial
plexus (Pancoast syndrome). Distant metastases most commonly involve the brain,
bone, liver, and adrenal glands.
Treatment
Surgery is the treatment of choice to
reduce the tumor burden in nonmetastatic lung cancer. Various chemotherapy and radiation
treatments are likewise employed, but there is wide variation among tis-sue
types in their sensitivity to chemotherapy and radiation.
Resectability & Operability
Resectability is determined by the
anatomic stage of the tumor, whereas operability is dependent on the
interaction between the extent of the procedure required for cure and the
physiological status of the patient. Anatomic staging is accomplished using
chest radiography, computed tomography (CT) or magnetic resonance imaging
(MRI), bronchoscopy, and (sometimes) mediastinoscopy. The extent of the surgery
should maximize the chances for a cure but still allow for adequate residual
pulmonary function postoperatively. Lobectomy via a posterior thora-cotomy,
through the fifth or sixth intercostal space, or thorough video assisted
thoracoscopic surgery (VATS), is the procedure of choice for most lesions.
Segmental or wedge resections may be performed in patients with small
peripheral lesions and poor pul-monary reserve. Pneumonectomy is necessary for
curative treatment of lesions involving the left or right main bronchus or when
the tumor extends toward the hilum. A sleeve resection may be employed for
patients with proximal lesions and limited pulmonary reserve as an alternative
to pneumonectomy; in such instances, the involved lobar bronchus, together with
part of the right or left main bronchus, is resected, and the distal bronchus
is reanastomosed to the proximal bronchus or the trachea. Sleeve pneumonectomy
may be considered for tumors involving the trachea.
The incidence of pulmonary complications
after thoracotomy and lung resection is about 30% and is related not only to
the amount of lung tis-sue resected, but also to the disruption of chest wall
mechanics due to the thoracotomy. Postoperative pulmonary dysfunction seems to
be less after VATS than “open”
thoracotomy. The mortality rate for pneumonectomy is generally more than twice
that of for a lobectomy. Mortality is greater for right-sided than left-sided
pneumonectomy, possibly because of greater loss of lung tissue.
Evaluation for Lung Resection
A comprehensive preoperative pulmonary
assess-ment is necessary to assess the operative risk, minimize perioperative
complications, and achieve better outcomes. Preoperative assessment of
respi-ratory function includes determinations of respira-tory mechanics, gas
exchange, and cardiorespiratory interaction.Respiratory mechanics are assessed
by pulmo-nary function tests. Of these parameters, the most useful is the
predicted postoperative forced expira-tory volume in one sec (FEV1), which is calculated as follows:
Postoperative FEV1 = preoperative FEV1 × (1 – the percentage of functional lung tissue
removed divided by 100)
Removal of extensively diseased lung
(nonven-tilated but perfused) does not necessarily adversely affect pulmonary
function and may actually improve oxygenation. Mortality and morbidity are
signifi-cantly increased if postoperative FEV1 is less than 40% of normative FEV1, and patients with predicted postoperative FEV1 of less than 30% may need post-operative mechanical
ventilatory support.Gas exchange will sometimes be characterized by diffusion
lung capacity for carbon monoxide (DLCO). DLCO correlates with the total
function-ing surface area of the alveolar–capillary interface. Predictive
postoperative DLCO can be calculated in the same fashion as postoperative FEV1. A predicted postoperative DLCO of less than 40%
also corre-lates with increased postoperative respiratory and cardiac
complications. Adequacy of gas exchange is more commonly assessed by
arterialblood gas data such as Pao2 >60 mm Hg and· a Pa·co2 <45 mm Hg.
Ventilation-perfusion(V/Q)scintigraphy
pro-vides the relative contribution of each lobe to over-all pulmonary function
and may further refine the assessment of predicted postoperative lung function,
in patients where pneumonectomy is the indicated surgical procedure and there
is concern whether a single lung will be adequate to support life.
Patients considered at greater risk of
periop-erative complications based on standard spirometry testing and
calculation of postoperative function should undergo exercise testing for
evaluation of
cardiopulmonary interaction. Stair
climbing is the easiest way to assess exercise capacity and cardio-pulmonary
reserve. Patients capable of climbing two or three flights of stairs have
decreased mortal-ity and morbidity. On the other hand, the ability to climb
less than two flights of stairs is associated with increased perioperative
risk. The gold standard for evaluating cardiopulmonary interaction is by
labo-ratory exercise testing and measurement of maximal minute oxygen consumption.
A V˙o2>20 mL/kg is not associated with a significant increase in
peri-operative mortality or morbidity, whereas a minute consumption of less
than 10 mL/kg is associated
with an increased perioperative risk.
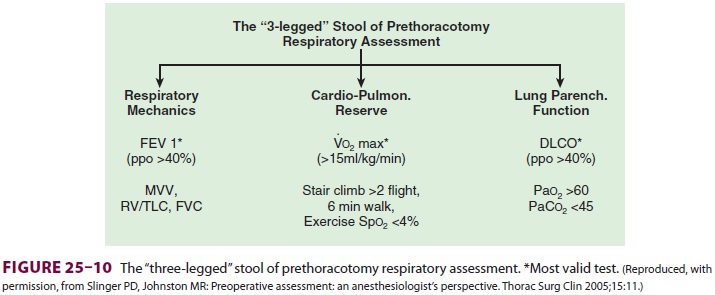
A combination of tests to evaluate the
three components of the respiratory function (ie, respira-tory mechanics, gas
exchange, and cardiopulmonary interaction) has been summarized in the so-called
“three-legged” stool of respiratory assessment (Figure25–10).
2. Infection
Pulmonary infections may present as a
solitary nod-ule or cavitary lesion (necrotizing pneumonitis). An exploratory
thoracotomy may be carried out to exclude malignancy and diagnose the
infectious agent. Lung resection is also indicated for cavitary lesions that
are refractory to antibiotic treatment, are associated with refractory empyema,
or result inmassive hemoptysis. Responsible organisms include both bacteria and
fungi.
3. Bronchiectasis
Bronchiectasis is a permanent dilation
of bronchi. It is usually the end result of severe or recurrent inflammation
and obstruction of bronchi. Causes include a variety of viral, bacterial, and
fungal patho-gens, as well as inhalation of toxic gases, aspiration of gastric
acid, and defective mucociliary clearance (cystic fibrosis and disorders of ciliary
dysfunction). Bronchial muscle and elastic tissue are typically replaced by
very vascular fibrous tissue. The lat-ter predisposes to bouts of hemoptysis.
Pulmonary resection is usually indicated for massive hemopty-sis when
conservative measures have failed and the disease is localized. Patients with
diffuse bronchiec-tasis have a chronic obstructive ventilatory defect.
Related Topics