Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Thoracic Surgery
Techniques for One-Lung Ventilation
Techniques for One-Lung Ventilation
One-lung ventilation can also be
utilized to isolate a lung or to facilitate ventilatory management under
certain conditions (Table25–1). Three techniques can be employed: (1)
placement of a double-lumen
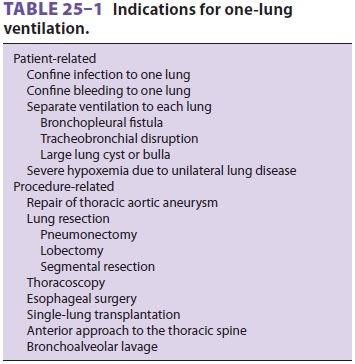
bronchial tube; (2) use of a
single-lumen tracheal tube in conjunction with a bronchial blocker; or
insertion of a conventional endotracheal tube into a mainstem bronchus.
Double-lumen tubes are most often used.
DOUBLE LUMEN BRONCHIAL TUBES
The principal advantages of double-lumen
tubes are relative ease of placement, the ability to ventilate one or both
lungs, and the ability to suction either lung.
All double-lumen tubes share the
following characteristics:
·
A
longer bronchial lumen that enters either the right or left main bronchus and
another shorter tracheal lumen that terminates in the lower trachea
·
A
preformed curve that when properly “aimed” allows preferential entry into
abronchus
·
A
bronchial cuff
·
A
tracheal cuff
Ventilation can be delivered to only one
lungby clamping either the bronchial or tracheal lumen with both cuffs
inflated; opening the port on the appropriate connector allows the ipsilateral
lung to collapse. Because of differences in bronchial anatomy between the two
sides, tubes are designed specifically for either the right or left bronchus. A
right-sided double-lumen tube incorporates a modi-fied cuff and a proximal
portal on the endobronchial side for ventilation of the right upper lobe. The
most commonly used double-lumen tube are available in several sizes: 35, 37,
39, and 41F.
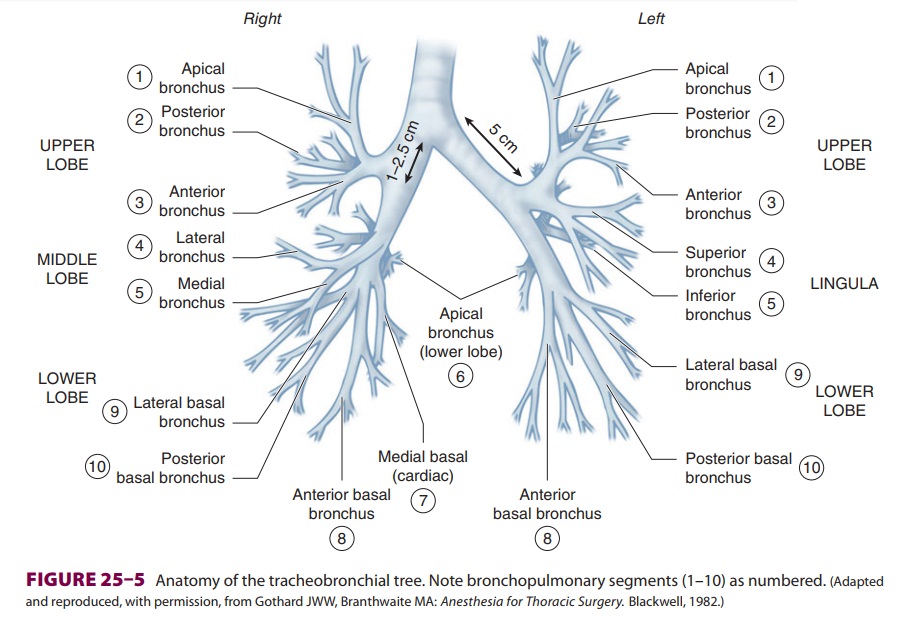
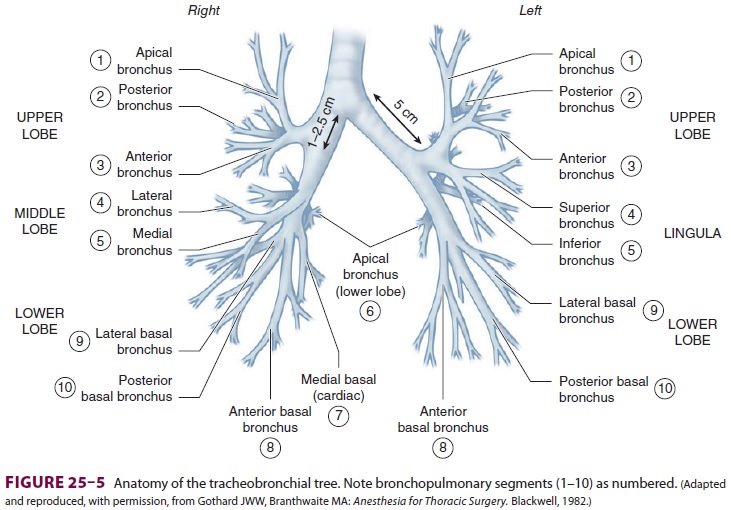
Anatomic Considerations
On average, the adult trachea is 11–13
cm long. It begins at the level of the cricoid cartilage (C6) and bifurcates at
the level of the carina behind the ster-nomanubrial joint (T5). Major
differences between the right and left main bronchi are as follows:
the larger diameter right bronchus
diverges away from the trachea at a less acute angle in relation to the
trachea, whereas the left bronchus diverges at a more horizontal angle ( Figure25–5);
(2) the right bronchus has upper, middle, and lower lobe branches, whereas the
left bronchus divides into only upper and lower lobe branches; and (3) the
orifice of the right upper lobe bronchus is typically about 1–2.5 cm from the
carina, whereas the bifurcation of the left main bronchus is typically about 5
cm distal to the carina. There is considerable anatomic varia-tion: for
example, the right upper lobe bronchus will occasionally arise from the trachea
itself.
As previously noted, right-sided
double-lumen tubes must have a portal through the bronchial cuff for
ventilating the right upper lobe ( Figure25–6). Anatomic variations among individuals
in the dis-tance between the carina and the right upper lobe orifice will
occasionally result in difficulty ventilating that lobe with right-sided tubes.
A left-sided double-lumen tube can be used in most surgical
procedures,irrespective of the operative side. There are certain clinical
situations in which the use ofa right-sided double-lumen tube is recommended:
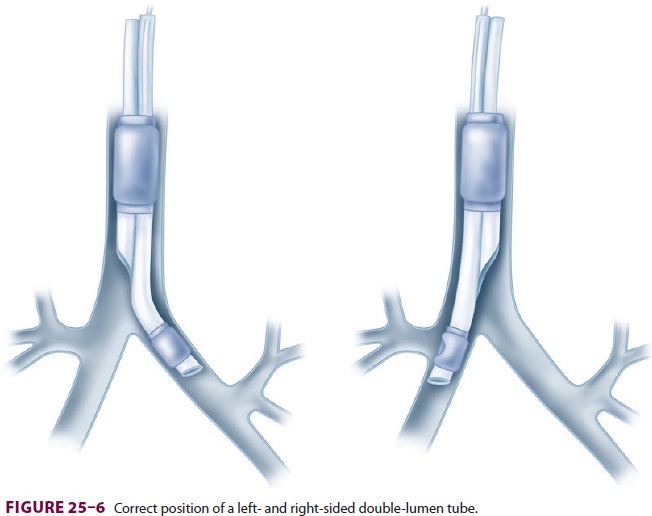
distorted anatomy of the left main
bronchus by an intrabronchial or extrabronchial mass; (2) compres-sion of the
left main bronchus due to a descending thoracic aortic aneurysm; (3) left-sided
pneumonec-tomy; (4) left-sided single lung transplantation; andleft-sided
sleeve resection. Finally, despite con-cerns about right upper lobe atelectasis
and poten-tially difficult placement, studies have failed to detect differences
in clinical performance of right- and left-sided double-lumen tubes when used
clinically.
Placement of Double-Lumen Tubes
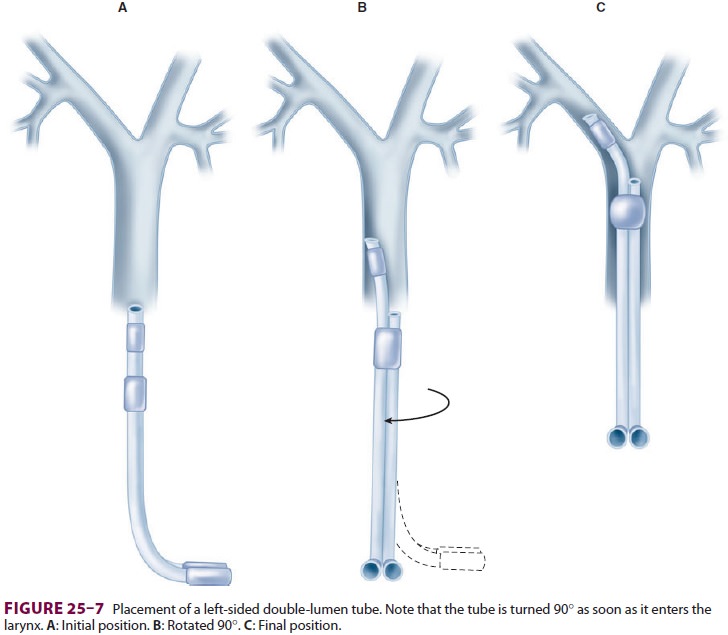
Laryngoscopy with a curved (MacIntosh)
blade usu-ally provides better intubating conditions than does a straight blade
because the curved blade typically pro-vides more room for manipulation of the
large double-lumen tube. Video laryngoscopy can also be employed to facilitate
tube placement. The double-lumen tube is passed with the distal curvature
concave anteriorly and is rotated 90°
(toward the side of the bronchus to be intubated) after the tip passes the
vocal cords and enters the larynx (Figure25–7). At this point, the operator has two
options: the tube can be advanced until resistance is felt (the average depth
of insertion is about 29 cm [at the teeth]), or alternatively, the fiber-optic
bronchoscope can be inserted through the bron-chial limb and advanced into the
desired bronchus. The double-lumen tube can be advanced over the bronchoscope
into the desired bronchus. Correct tube placement should be established using a
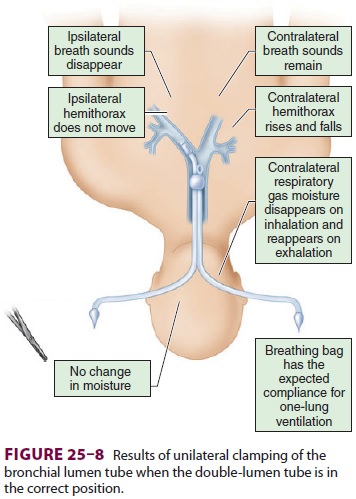
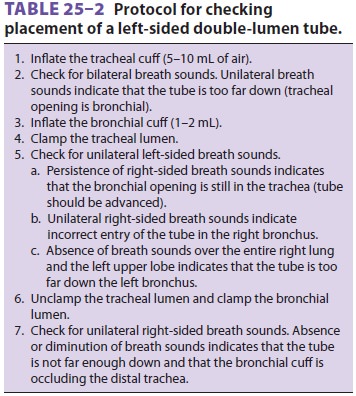
preset proto-col (Figure25–8 and Table25–2) and confirmed by flexible fiberoptic
bronchoscopy. When problems are encountered in intubating the patient with the
dou-ble-lumen tube, placement of a single-lumen endo-tracheal tube should be
attempted; once positioned in the trachea, the latter can be exchanged for the
dou-ble-lumen tube by using a specially designed catheter guide (“tube
exchanger”).
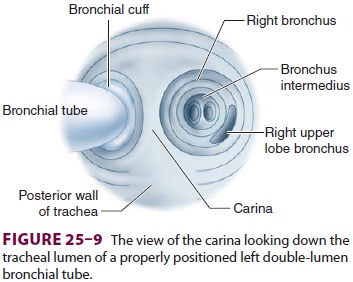
Most double-lumen tubes easily accommodate
bronchoscopes with a 3.6- to 4.2-mm outer diam-eter. When the bronchoscope is
introduced into the tracheal lumen and advanced through the tracheal orifice,
the carina should be visible (Figure25–9), and the bronchial limb of the tube
should be seen entering the respective bronchus; additionally, the top of the
bronchial cuff (usually colored blue) should be visible, but should not extend
above the carina. If the bronchial cuff of a left-sided double-lumen tube is
not visible, the bronchial limb may have been inserted sufficiently far to
allow the bron-chial cuff to obstruct the orifice of the left upper or lower
lobe; the tube should be withdrawn until the cuff can be identified distal to
the carina. The opti-mal position of a right-sided double-lumen tube is
confirmed by placing the fiberoptic scope through the endobronchial lumen,
which should show alignment of the endobronchial side portal with the opening
of the right upper lobe bronchus. The bronchial cuff should be inflated only to
the point at which the audible leak from the open tracheal lumen disappears
while ventilating only through the bron-chial lumen. Tube position should be
reconfirmed after the patient is positioned for surgery because the tube may
move relative to the carina as the patient is turned into the lateral decubitus
position. Malpositioning of a double-lumen tube is usually
the tube is in the right bronchus (the
wrong side). If the tube tip is located too distally, the bronchial cuff can
obstruct the left upper or the left lower lobe orifice, and the bronchial lumen
can be inserted into the orifice of the left lower or left upper lobe bronchus,
respectively. When the tube is not advanced distally enough, the inflated
bron-chial cuff may be above the carina and also occlude the tracheal lumen. In
both instances, deflation of the bronchial cuff improves ventilation to the
lung and helps to identify the problem. In some patients, the bronchial lumen
may be within the left upper or left lower lobe bronchus but with the tracheal
opening remaining above the carina; this situation is suggested by collapse of
only one of the left lobeswhen the bronchial lumen is clamped. In the same
situation, if the surgical procedure is in the right thorax, clamping of the
tracheal lumen will lead to ventilation of only the left upper or left lower
lobe; hypoxia usually develops rapidly.
Right-sided double-lumen tubes can be acci-dentally inserted into the left main stem bronchus, inserted too distally or too proximally, or have misalignment of the endobronchial side portal with the opening of the right upper lobe bronchus. If the tube inadvertently enters the wrong bronchus, the fiberoptic bronchoscope can be used to direct it into the correct side: (1) the bronchoscope is passed through the bronchial lumen to the tip of the tube;
under direct vision, the tube and the
broncho-scope are withdrawn together into the trachea just above the carina; (3)
the bronchoscope alone is then advanced into the correct bronchus; and (4) the
double-lumen tube is gently advanced over the bron-choscope, which functions as
a stylet to guide the bronchial lumen into the correct bronchus.
Complications of Double-Lumen Tubes
Major complications of double-lumen
tubes include:
hypoxemia due to tube malplacement, tube
occlusion, or excessive degrees of venous admixture with one-lung ventilation;
(2) traumatic laryngitis;
tracheobronchial rupture resulting from
trau-matic placement or overinflation of the bronchial cuff; and (4)
inadvertent suturing of the tube to a bronchus during surgery (detected as the
inability to withdraw the tube during attempted extubation).
SINGLE LUMEN TRACHEAL TUBES WITH A BRONCHIAL BLOCKER
Bronchial blockers are inflatable
devices that are passed alongside or through a single-lumen tracheal tube to
selectively occlude a bronchial orifice. A single-lumen tracheal tube with a
built-in side chan-nel for a retractable bronchial blocker is available. The
tube is placed with the blocker fully retracted; its natural curve is such that
turning the tube with the curve concave toward the right preferentially directs
the bronchial blocker toward the right bronchus. Turning the tube with the
curve concave toward the left usually directs the blocker toward the left
bron-chus. The bronchial blocker must be advanced, posi-tioned, and inflated
under direct visualization via a flexible bronchoscope.
The major advantage of a tube with an
incorpo-rated bronchial blocker is that, unlike a double-lumen tube, it does not need to be replaced
with a conven-tional tracheal tube if the patient remains intubated
postoperatively (below). Its major disadvantage is that the “blocked” lung
collapses slowly (and some-times incompletely) because of the small size of the
channel within the blocker.
Another way to achieve lung separation
is by using an independent bronchial blocker passed through a single-lumen
endotracheal tube. There are several types of independent bronchial blockers.
They come in different sizes (7Fr and 9Fr) and have a 1.4-mm diameter inner
lumen. Bronchial block-ers have a high-volume low-pressure cuff with either an
elliptical or spherical shape. The spherical shape of the cuff facilitates
adequate blockade of the right mainstem bronchus. The spherical or the
elliptical cuff can be used for the left main stem bronchus. The inner lumen
contains a nylon wire, which exits the distal end as a wireloop. The placement
of the bronchial blocker involves inserting the endobron-chial blocker through
the endotracheal tube and using the fiberoptic bronchoscope and the distal loop
of the guidewire to direct the blocker into a mainstem bronchus. The fiberoptic
bronchoscope must be advanced beyond the bronchus opening so that the blocker
enters the bronchus while it is being advanced. When the deflated cuff is
beyond the entrance of the bronchus, the fiberoptic bron-choscope is withdrawn,
and the blocker is secured in position. In order to obtain bronchial blockade,
the cuff is fully inflated under fiberoptic visualiza-tion with 4 to 8 mL of
air. The placement must be reconfirmed when the patient is placed in the
lateral position. Bronchial blockers may be good choices for lung separation in
intubated critically ill patients who require one-lung ventilation, patients
who are difficult to intubate using direct laryngoscopy, patients with prior
tracheostomies, and patients who may require postoperative mechanical
ven-tilation. However, because bronchial blockers are more prone to dislodgement
compared with double-lumen endotracheal tubes, and their small central lumens
do not allow efficient suctioning of secre-tions or rapid collapse of the lung,
some clinicians prefer not to use them.
In smaller children, an inflatable
embolec-tomy (Fogarty) catheter can be used as a bronchialblocker in
conjunction with a conventional tracheal tube (with the embolectomy catheter
placed either inside or alongside the tracheal tube); a guidewire in the
catheter can be used to facilitate placement. This technique is occasionally
used to collapse one lung when other techniques do not work. As the embolectomy
catheter does not have a communi-cating channel in the center, it also does not
allow suctioning or ventilation of the isolated lung, and the catheter can be
easily dislodged. Nonetheless, such bronchial blockers may be useful for
one-lung anesthesia in pediatric patients and for tamponad-ing bronchial
bleeding in adult patients .
Related Topics