Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Thoracic Surgery
Anesthesia for Lung Transplantation
Anesthesia for Lung Transplantation
PREOPERATIVE CONSIDERATIONS
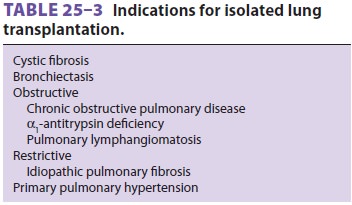
Lung transplantation is indicated for
end-stage pul-monary parenchymal disease or pulmonary hyper-tension. Candidates
are functionally incapacitated by dyspnea and have a poor prognosis. Criteria
vary according to the primary disease process. Common etiologies are listed in Table25–3.
Lung transplan-tation (as is true for all solid organ transplants) is limited
by the availability of suitable organs, not by the availability of recipients.
Patients typically have dyspnea at rest or with minimal activity and resting
hypoxemia (Pao2<50 mm Hg) with increasing oxy-gen requirements.
Progressive CO2 retention is also very common. Patients may be
ventilator depen-dent. Cor pulmonale does not necessarily require combined
heart–lung transplantation because right ventricular function may recover when
pulmonary artery pressures normalize. Patients should have normal left
ventricular function and be free of coro-nary artery disease, as well as other
serious health problems.
Single-lung transplantation may be
performed in selected patients with idiopathic pulmonary fibrosis, whereas
double-lung transplantation is typ-ically performed in patients with cystic
fibrosis, bul-lous emphysema, or vascular diseases. Patients with Eisenmenger
syndrome require combined heart– lung transplantation.
ANESTHETIC CONSIDERATIONS
1. Preoperative Management
Effective coordination between the
organ-retrieval team and the transplant team minimizes graft isch-emia time and
avoids unnecessary prolongation of pretransplant anesthesia time. These
procedures are performed on an emergency basis; therefore, patients may have
little time to fast for surgery. Oral cyclosporine also may be given
preoperatively. Administration of a clear antacid, an H2 blocker, or
metoclopramide should be considered. Patients are very sensitive to sedatives,
so premedication is usu-ally administered only in the operating room when the
patient is directly attended. Immunosuppressants and antibiotics are also
administered after induction and prior to surgical incision.
2. Intraoperative Management
Monitoring
Strict asepsis should be observed for
invasive moni-toring procedures. Central venous access might be accomplished
only after induction of anesthesia because patients may not be able to lie flat
while awake. Patients with a patent foramen ovale are at risk of paradoxical
embolism because of high right atrial pressures.
Induction & Maintenance of Anesthesia
A rapid-sequence induction is utilized.
Induction with ketamine, etomidate, an opioid, or a combina-tion of these
agents is employed, avoiding precipi-tous drops in blood pressure. An NMB is
used to facilitate laryngoscopy. Hypoxemia and hypercar-bia must be avoided to
prevent further increases in pulmonary artery pressure. Hypotension should be
treated with vasopressors instead of large fluid boluses .
Anesthesia is usually maintained with
total intravenous anesthesia or a volatile agent. Intra-operative difficulties
in ventilation are not uncom-mon. Progressive retention of CO2 can
also be a problem intraoperatively. Ventilation should be adjusted to maintain a Paco2
as close to the patient’s baseline as possible. However, in the presence of a
reasonable cardiovascular reserve and normal right heart function, higher
levels of Paco2 can be toler-ated for short periods of time.
Hypercarbia and aci-dosis may lead to pulmonary vasoconstriction and acute
right heart failure, and hemodynamic support with inotropes may be required for
these patients. Patients with cystic fibrosis have copious secretions and require
frequent suctioning.
Single-Lung Transplantation
Single-lung transplantation is often
attempted without CPB. The procedure is performed through a posterior
thoracotomy. Whether to employ CPB during transplantation of one lung is based
on the patient’s response to collapsing the lung to be replaced and clamping
its pulmonary artery. Persistent arterial hypoxemia (Spo2< 88%) or a sudden increase in pulmonary artery
pres-sures necessitates CPB. Prostaglandin E1,
mil-rinone, nitroglycerin, and dobutamine may be utilized to reduce pulmonary
hypertension and prevent right ventricular failure. Inotropic sup-port may be
necessary. After the recipient lung is removed, the pulmonary artery, left
atrial cuff (with the pulmonary veins), and bronchus of the donor lung are
anastomosed. Flexible bronchos-copy is used to examine the bronchial suture
line after its completion.
Double-Lung Transplantation
A “clamshell” transverse sternotomy can
be used for double-lung transplantation. The procedure is occa-sionally
performed with CPB; sequential thoracoto-mies for double-lung transplantation
can also be performed. Heart lung transplantation is performed through median
sternotomy with CPB.
Posttransplantation Management
After anastomosis of the donor organ or
organs, ventilation to both lungs is resumed. Following transplantation, peak
inspiratory pressuresshould be maintained at the minimum pressure compatible
with good lung expansion, and the inspired oxygen concentration should be
maintained as close to room air as allowed by a Pao2>60 mm Hg. Methylprednisolone and mannitol are
usually administered prior to the release of vascular clamps. Hyperkalemia may
occur as the preservative fluid is washed out of the donor organ. If
transplantation has been performed on CPB, the patient is separated from CPB.
Pulmonary vasodilators, inhaled nitric oxide, and inotropes (above) may be
necessary. Transesophageal echocardiography is helpful in dif-ferentiating
right and left ventricular dysfunction, as well as in evaluating blood flow in
the pulmonary vessels, particularly after transplantation.
Transplantation disrupts the neural
innerva-tion, lymphatic drainage, and bronchial circulation of the transplanted
lung. The respiratory pattern is unaffected, but the cough reflex is abolished
below the carina. Bronchial hyperreactivity is observed in some patients.
Hypoxic pulmonary vasoconstriction remains normal. Loss of lymphatic drainage
increases extravascular lung water and predisposes the trans-planted lung to
pulmonary edema. Intraoperative fluid replacement must therefore be kept to a
mini-mum. Loss of the bronchial circulation predisposes to ischemic breakdown
of the bronchial suture line.
3. Postoperative Management
Patients are extubated after surgery as
soon as is feasible. A thoracic epidural catheter may be employed for
postoperative analgesia when coagu-lation studies are normal. The postoperative
course may be complicated by acute rejection, infections, and renal and hepatic
dysfunction. Deteriorating lung function may result from rejection or
reperfu-sion injury. Occasionally, temporary extracorporeal membrane
oxygenation may be necessary. Frequent bronchoscopy with transbronchial
biopsies and lavage are necessary to differentiate between rejec-tion and
infection. Nosocomial Gram-negative bac-teria, cytomegalovirus, Candida, Aspergillus, and Pneumocystis carinii are common pathogens. Otherpostoperative surgical
complications include dam-age to the phrenic, vagus, and left recurrent
laryn-geal nerves.
Related Topics