Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Thoracic Surgery
Anesthesia for Tracheal Resection
Anesthesia for Tracheal Resection
Preoperative Considerations
Tracheal resection is most commonly
performed for tracheal stenosis, tumors, or, less commonly, con-genital
abnormalities. Tracheal stenosis can result from penetrating or blunt trauma,
as well as trachealintubation and tracheostomy. Squamous cell and adenoid
cystic carcinomas account for the major-ity of tumors. Compromise of the
tracheal lumen results in progressive dyspnea. Wheezing or stridor may be
evident only with exertion. The dyspnea may be worse when the patient is lying
down, with progressive airway obstruction. Hemoptysis can also complicate
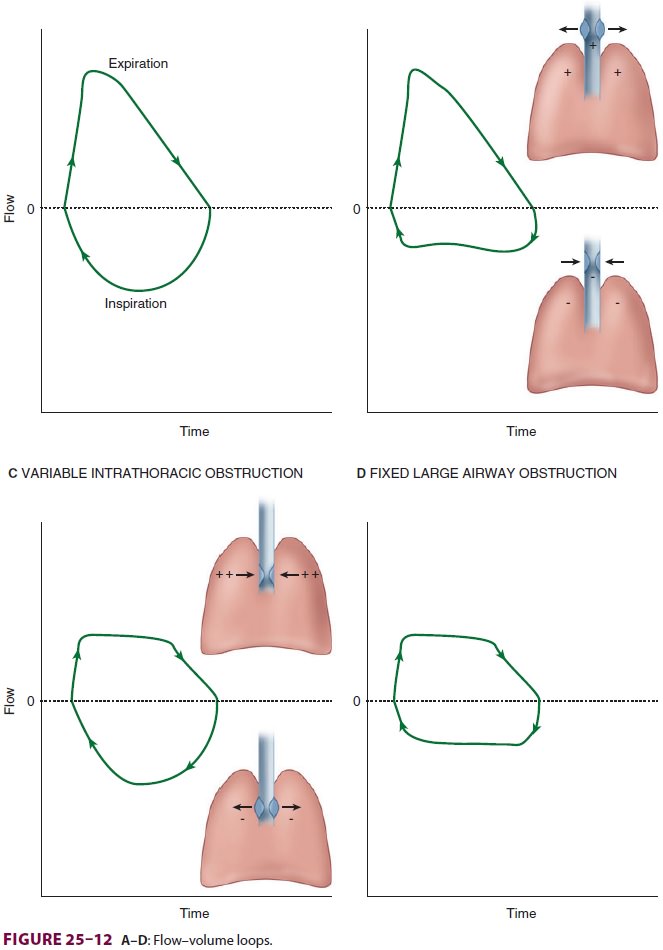
tracheal tumors. CT is valuable in localizing the lesion. Measurement of flow–volumeloops
confirms the location of the obstruction and aids the clinician in evaluating the severity of the lesion (Figure25–12).
Anesthetic Considerations
Little premedication is given, as most
patients pre-senting for tracheal resection have moderate to severe airway
obstruction. Use of an anticholinergic agent to dry secretions is controversial
because of the theoretical risk of inspissation. Monitoring should include
direct arterial pressure measurements.
An inhalation induction (in 100% oxygen)
is carried out in patients with severe obstruction. Sevoflurane is preferred
because it is the potent anesthetic that is least irritating to the airway.
Spontaneous ventilation is maintained throughout induction. NMBs are generally
avoided because of the potential for complete airway obstruction follow-ing
neuromuscular blockade. Laryngoscopy is per-formed only when the patient is
judged to be under deep anesthesia. Intravenous lidocaine (1–2 mg/kg) can deepen the anesthesia without
depressing respi-rations. The surgeon may then perform rigid bron-choscopy to
evaluate and possibly dilate the lesion. Following bronchoscopy, the patient is
intubated with a tracheal tube small enough to be passed distal to the
obstruction whenever possible.
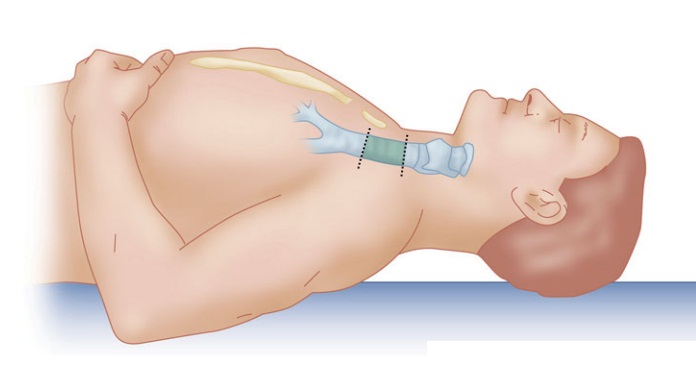
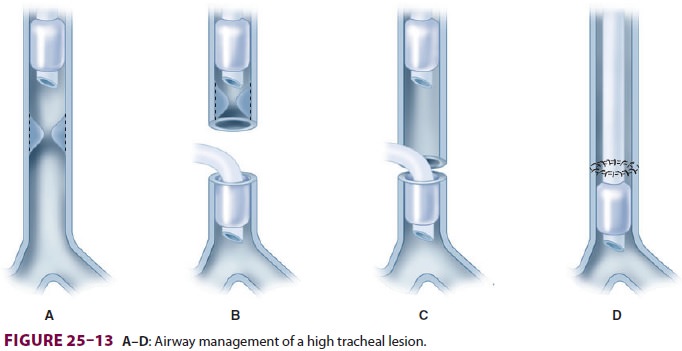
A collar incision is utilized for high
tracheal lesions. The surgeon divides the trachea in the neck and advances a
sterile armored tube into the distal trachea, passing off a sterile connecting
breathing circuit to the anesthesiologist for ventilation during the resection.
Following the resection and comple-tion of the posterior part of the
reanastomosis, the armored tube is removed, and the original tracheal tube is
advanced distally, past the anastomosis (Figure25–13). Alternatively, high-frequency jet
ventilation may be employed during the anastomosis
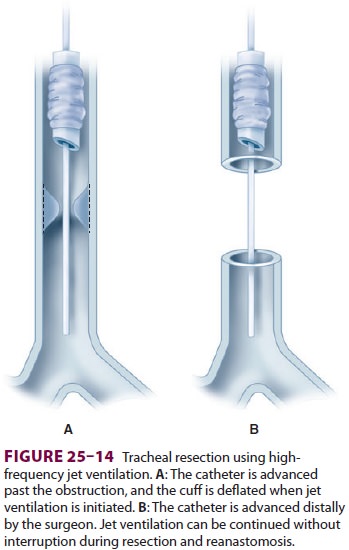
by passing the jet cannula past the
obstruction and into the distal trachea ( Figure25–14). Return of spontaneous ventilation and
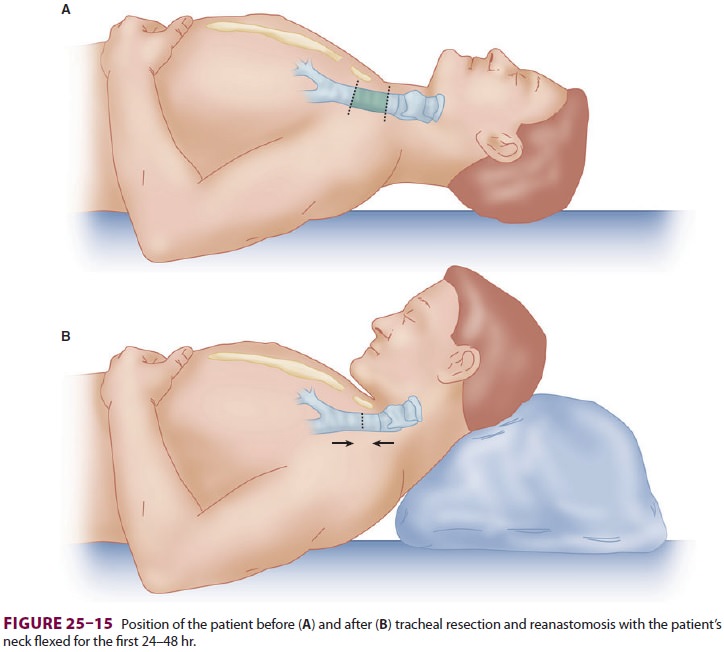
early extubation at the end of the procedure are desirable. Patients should be
positioned with the neck flexed immediately after the operation to minimize
tension on the suture line (Figure25–15).
Surgical management of low tracheal
lesions requires a median sternotomy or right posterior thoracotomy. Anesthetic
management is similar, but more regularly requires more complicated tech-niques,
such as high-frequency ventilation or even cardiopulmonary bypass (CPB) in
complex congen-ital cases.
Related Topics