Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Thoracic Surgery
Physiological Considerations During Thoracic Anesthesia
Physiological Considerations During Thoracic Anesthesia
Thoracic surgery presents a unique set
of physiologi-cal problems for the anesthesiologist. These include
physiological derangements caused by placing the patient in the lateral
decubitus position, opening the chest (open
pneumothorax), and the need for one-lung ventilation.
THE LATERAL DECUBITUS POSITION
The lateral decubitus position provides
optimal access for most operations on the lungs, pleura, esophagus, the great
vessels, other mediastinal structures, and vertebrae. Unfortunately, this
posi-tion may significantly alter the normal pulmonary ventilation/perfusion relationships. These
derange-ments are further accentuated by induction of anesthesia, initiation of
mechanical ventilation, neu-romuscular blockade, opening the chest, and
surgical retraction. Although perfusion continues to favor the dependent
(lower) lung, ventilation progressively favors the less perfused upper lung.
The resulting mismatch increases the risk of hypoxemia.
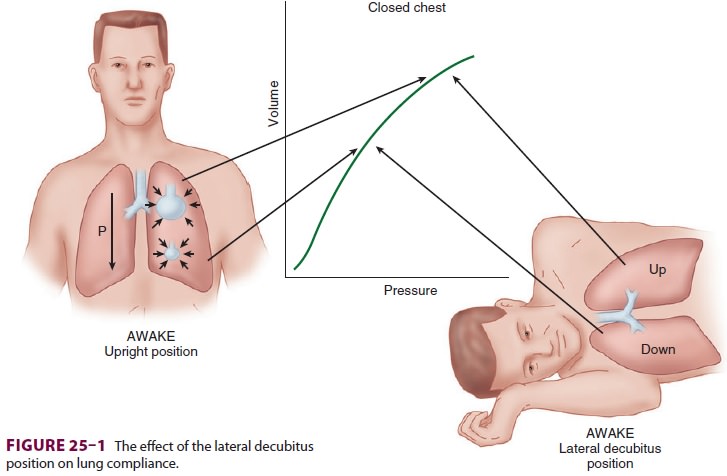
The Awake State
When a supine patient assumes the
lateral decu-bitus position, ventilation/perfusion matching is preserved during
spontaneous ventilation. The dependent (lower) lung receives more perfusion
than does the upper lung due to gravitational influ-ences on blood flow
distribution in the pulmonary circulation. The dependent lung also receives
more ventilation because: (1) contraction of the depen-dent hemidiaphragm is
more efficient compared with the nondependent [upper] hemidiaphragm and (2) the
dependent lung is on a more favorable part of the compliance curve ( Figure25–1).
Induction of Anesthesia
The decrease in functional residual
capacity (FRC) with induction of general anesthesia moves the upper lung to a
more favorable part of the compliance
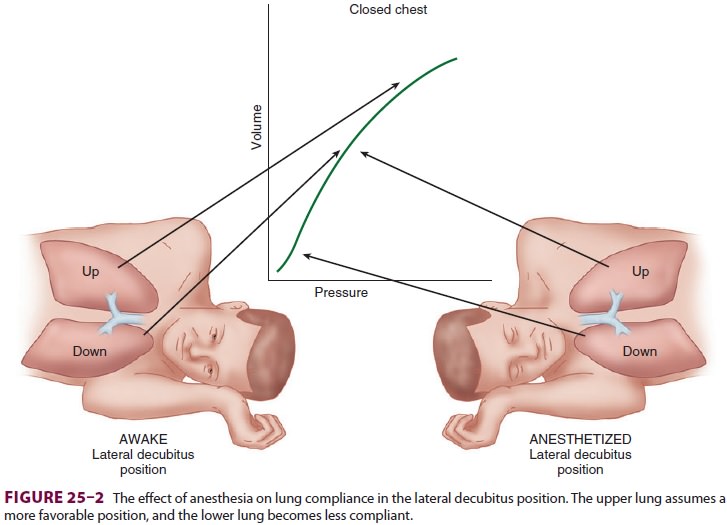
curve, but moves the lower lung to a
less favorable-position (Figure25–2). As a result, the upper lung is
ventilated more than the dependent lower lung; ven-tilation/perfusion mismatching occurs because the
dependent lung continues to have greater perfusion.
Positive-Pressure Ventilation
Controlled positive-pressure ventilation
favors the upper lung in the lateral position because it is more compliant than
the lower lung. Neuromuscular blockade enhances this effect by allowing the
abdominal contents to rise up further against the dependent hemidiaphragm and
impede ventila-tion of the lower lung. Using a rigid “bean bag” to maintain the
patient in the lateral decubitus position further restricts movement of the
dependent hemi-thorax. Finally, opening the nondependent side of the chest
further accentuates differences in compli-ance between the two sides because
the upper lung is now less restricted in movement. All of these effectsworsen
ventilation/perfusion
mismatching and pre-dispose the patient to hypoxemia.
THE OPEN PNEUMOTHORAX
The lungs are normally kept expanded by
a negative pleural pressure—the net result of the tendency of the lung to
collapse and the chest wall to expand. When one side of the chest is opened,
the negative pleural pressure is lost, and the elastic recoil of the lung on
that side tends to collapse it. Spontaneous ventilation with an open
pneumothorax in the lateral position results in paradoxical respirations and
mediastinal shift. These two phenomena can cause progressive hypox-emia and
hypercapnia, but, fortunately, their effects are overcome by the use of
positive-pressure ventila-tion during general anesthesia and thoracotomy.
Mediastinal Shift
During spontaneous ventilation in the
lateral posi-tion, inspiration causes pleural pressure to become
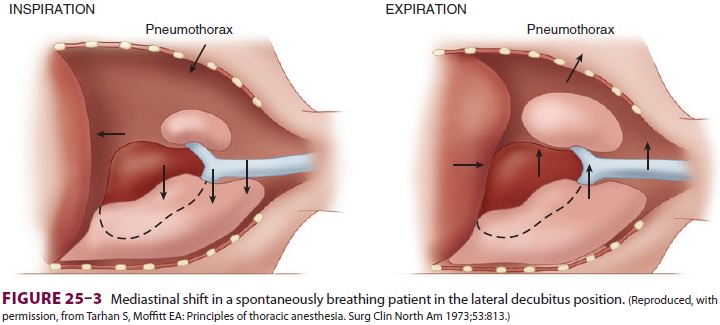
more negative on the dependent side, but
not on the side of the open pneumothorax. This results in a downward shift of
the mediastinum during inspiration and an upward shift during expiration (Figure25–3).
The major effect of the mediastinal shift is to decrease the contribution of
the dependent lung to the tidal volume.
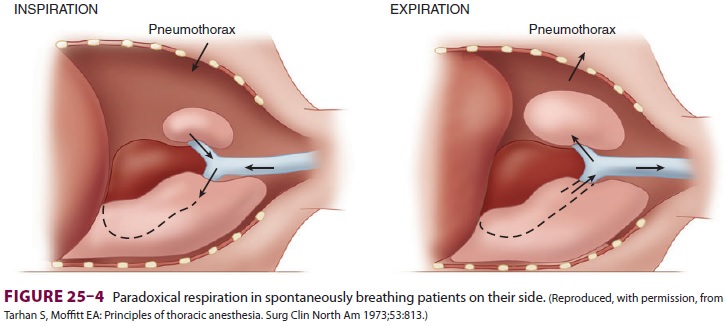
Paradoxical Respiration
Spontaneous ventilation in a patient
with an open pneumothorax also results in to-and-fro gas flow between the
dependent and nondependent lung(paradoxical respiration [pendeluft]). During
inspi-ration, the pneumothorax increases, and gas flows from the upper lung
across the carina to the depen-dent lung. During expiration, the gas flow reverses
and moves from the dependent to the upper lung (Figure 25–4).
ONE LUNG VENTILATION
Intentional collapse of the lung on the operative side facilitates most thoracic procedures, but greatly complicates anesthetic management. Because the collapsed lung continues to be perfused and is delib-erately no longer ventilated, the patient develops a large right-to-left intrapulmonary shunt (20% to 30%). During one-lung ventilation, the mixing of unoxygenated blood from the collapsedupper lung with oxygenated blood from the still-ventilated dependent lung widens the alveolar-to-arterial (A-a) O2 gradient and often results in hypoxemia. Fortunately, blood flow to the nonventi-lated lung is decreased by hypoxic pulmonary vaso-constriction (HPV) and possibly surgical compression of the upper lung
Factors known to inhibit HPV (increasing venous admixture), and thus
worsen the right-to-left shunting, include (1) very high or very low pulmo-nary
artery pressures; (2) hypocapnia; (3) high or very low mixed venous Po2; (4) vasodilators such as nitroglycerin,
nitroprusside, phosophodiesterase inhibitors (milrinone and inamrinone),
β-adrenergic agonists, calcium channel blockers; (5) pulmonary infection; and
(6) inhalation anesthetics.
Factors that decrease blood flow to the
venti-lated lung can be equally detrimental; they counter-act the effect of HPV by indirectly increasing blood flow to
the collapsed lung. Such factors include
high mean airway pressures in the
ventilated lung due to high positive end-expiratory pressure (PEEP),
hyperventilation, or high peak inspiratory pressures;a low Fio2, which produces hypoxic pulmonary vasoconstriction
in the ventilated lung; (3) vasocon-strictors that may have a greater effect on
normoxic vessels than hypoxic ones; and (4) intrinsic PEEP that develops due to
inadequate expiratory times.Elimination of CO2 is usually unchanged
by one-lung ventilation, provided that minute ventila-tion is unchanged and
that preexisting CO 2 retention was not present while ventilating
both lungs; arterial CO2 tension is usually not appreciably altered.
Related Topics