Chapter: Basic & Clinical Pharmacology : Agents Used in Cardiac Arrhythmias
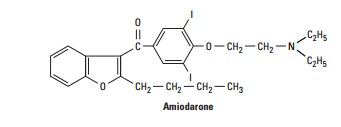
Amiodarone
AMIODARONE
In
the USA, amiodarone is approved for oral and intravenous use to treat serious
ventricular arrhythmias. However, the drug is also highly effective for the
treatment of supraventricular arrhythmias such as atrial fibrillation. As a
result of its broad spectrum of anti-arrhythmic action, it is very extensively
used for a wide variety of arrhythmias. Amiodarone has unusual pharmacokinetics
and impor-tant extracardiac adverse effects. Dronedarone, an analog that lacks iodine atoms, recently received
Food and Drug Administration approval for the treatment of atrial flutter and
fibrillation. Celivarone is another
noniodinated benzofuran derivative similar to drone-darone that is currently
undergoing clinical trials for the preven-tion of ventricular tachycardia
recurrence.
Cardiac Effects
Amiodarone
markedly prolongs the action potential duration (and the QT interval on the
ECG) by blockade of IKr. During chronic administration, IKs
is also blocked. The action potential duration is prolonged uniformly over a
wide range of heart rates; that is, the drug does not have reverse
use-dependent action. In spite of its present classification as a class 3
agent, amiodarone also signifi-cantly blocks inactivated sodium channels. Its
action potential-prolonging action reinforces this effect. Amiodarone also has
weak adrenergic and calcium channel-blocking actions. Consequences of these
actions include slowing of the heart rate and AV node conduction. The broad
spectrum of actions may account for its relatively high efficacy and its low
incidence of torsades de pointes despite significant QT-interval prolongation.
Extracardiac Effects
Amiodarone
causes peripheral vasodilation. This action is promi-nent after intravenous
administration and may be related to the action of the vehicle.
Toxicity
Amiodarone
may produce symptomatic bradycardia and heart block in patients with
preexisting sinus or AV node disease. The drug accumulates in many tissues,
including the heart (10–50 times more so than in plasma), lung, liver, and
skin, and is concentrated in tears. Dose-related pulmonary toxicity is the most
important adverse effect. Even on a low dose of 200 mg/d or less, fatal
pulmonary fibrosis may be observed in 1% of patients.
Abnormal
liver function tests and hypersensitivity hepatitis may develop during
amiodarone treatment and liver function tests should be monitored regularly.
The skin deposits result in a pho-todermatitis and a gray-blue skin
discoloration in sun-exposed areas, eg, the malar regions. After a few weeks of
treatment, asymptomatic corneal microdeposits are present in virtually all
patients treated with amiodarone. Halos develop in the peripheral visual fields
of some patients. Drug discontinuation is usually not required. Rarely, an
optic neuritis may progress to blindness.
Amiodarone
blocks the peripheral conversion of thyroxine (T4) to
triiodothyronine (T3). It is also a potential source of large
amounts of inorganic iodine. Amiodarone may result in hypothy-roidism or
hyperthyroidism. Thyroid function should be evaluated before initiating
treatment and should be monitored periodically. Because effects have been
described in virtually every organ system, amiodarone treatment should be
reevaluated whenever new symp-toms develop in a patient, including arrhythmia
aggravation.
Pharmacokinetics
Amiodarone
is variably absorbed with a bioavailability of 35–65%. It undergoes hepatic
metabolism, and the major metabolite, des-ethylamiodarone, is bioactive. The
elimination half-life is com-plex, with a rapid component of 3–10 days (50% of
the drug) and a slower component of several weeks. After discontinuation of the
drug, effects are maintained for 1–3 months. Measurable tissue levels may be
observed up to 1 year after discontinuation. A total loading dose of 10 g is
usually achieved with 0.8–1.2 g daily doses. The maintenance dose is 200–400 mg
daily. Pharmacologic effects may be achieved rapidly by intravenous loading.
QT-prolonging effect is modest with this route of administration, whereas
brady-cardia and AV block may be significant.
Amiodarone
has many important drug interactions, and all medications should be reviewed
when the drug is initiated and when the dose is adjusted. Amiodarone is a
substrate for liver cyto-chrome CYP3A4, and its levels are increased by drugs
that inhibit this enzyme, eg, the histamine H2 blocker cimetidine.
Drugs that induce CYP3A4, eg, rifampin, decrease amiodarone concentration when
coadministered. Amiodarone inhibits several cytochrome P450 enzymes and may
result in high levels of many drugs, includ-ing statins, digoxin, and warfarin.
The dose of warfarin should be reduced by one third to one half following
initiation of amio-darone, and prothrombin times should be closely monitored.
Therapeutic Use
Low
doses (100–200 mg/d) of amiodarone are effective in main-taining normal sinus
rhythm in patients with atrial fibrillation. The drug is effective in the
prevention of recurrent ventricular tachycardia. It is not associated with an
increase in mortality in patients with coronary artery disease or heart
failure. In many centers, the implanted cardioverter-defibrillator (ICD) has
suc-ceeded drug therapy as the primary treatment modality for ven-tricular
tachycardia, but amiodarone may be used for ventricular tachycardia as adjuvant
therapy to decrease the frequency of uncomfortable cardioverter defibrillator
discharges. The drug increases the pacing and defibrillation threshold and
these devices require retesting after a maintenance dose has been achieved.
Related Topics