Chapter: Clinical Anesthesiology: Anesthetic Management: Airway Management
Airway Management: Anatomy
Airway Management
Expert airway management is an essential
skill in anesthetic practice.
ANATOMY
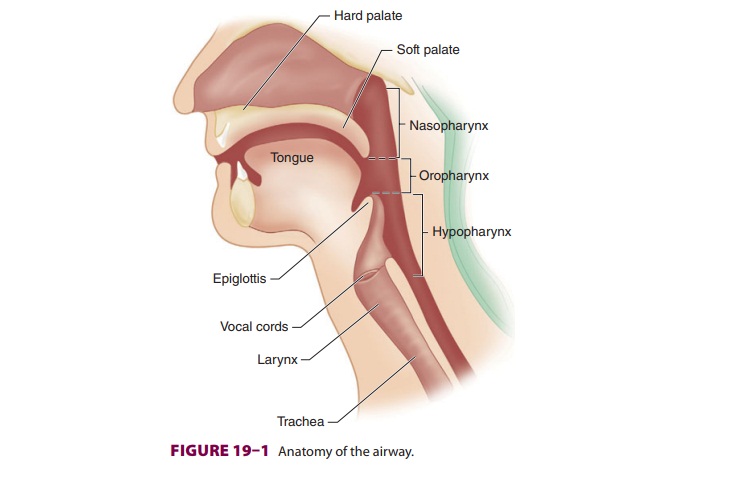
The upper airway consists of the
pharynx, nose, mouth, larynx, trachea, and main-stem bronchi. The mouth and
pharynx are also a part of the upper gas-trointestinal tract. The laryngeal
structures in part serve to prevent aspiration into the trachea.
There are two openings to the human
airway: the nose, which leads to the nasopharynx, and the mouth, which leads to
the oropharynx. These pas-sages are separated anteriorly by the palate, but
they join posteriorly in the pharynx ( Figure 19–1). The pharynx is a U-shaped
fibromuscular structure that extends from the base of the skull to the cricoid
car-tilage at the entrance to the esophagus. It opens ante-riorly into the
nasal cavity, the mouth, the larynx, and the nasopharynx, oropharynx, and
laryngo-pharynx, respectively. The nasopharynx is separated from the oropharynx
by an imaginary plane that extends posteriorly. At the base of the tongue, the
epiglottis functionally separates the orophar-ynx from the laryngopharynx (or
hypopharynx).
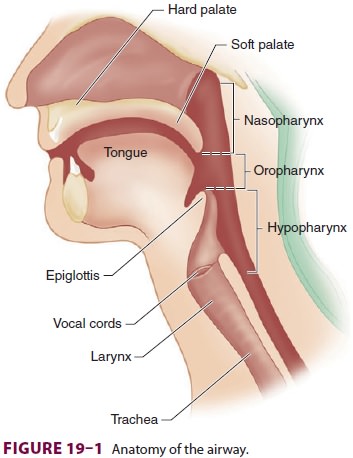
The epiglottis prevents aspiration by
covering the glottis—the opening of the larynx—during swal-lowing. The larynx
is a cartilaginous skeleton held together by ligaments and muscle. The larynx
is composed of nine cartilages ( Figure 19–2): thyroid, cricoid, epiglottic,
and (in pairs) arytenoid, cornicu-late, and cuneiform. The thyroid cartilage
shields the conus elasticus, which forms the vocal cords.
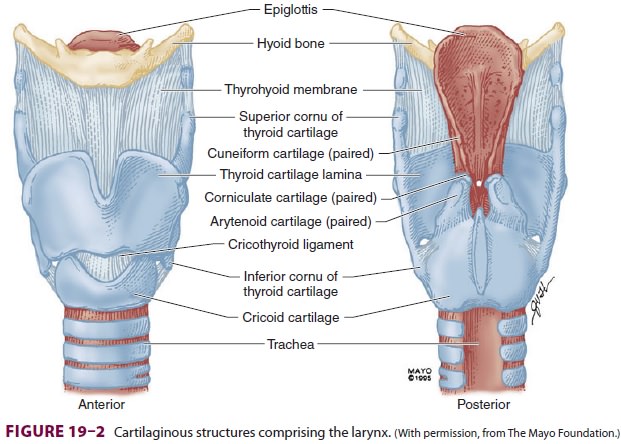
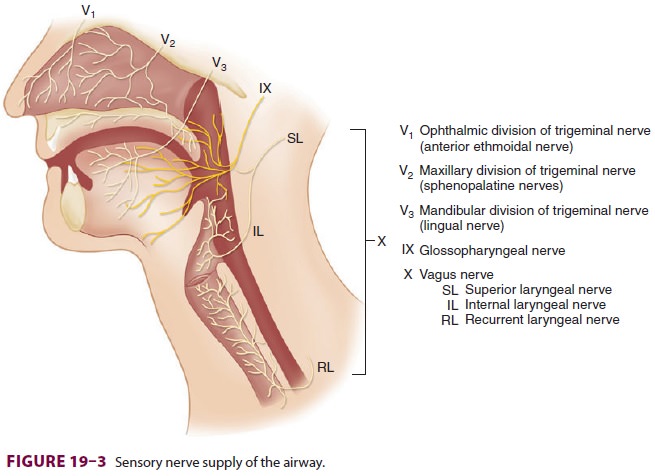
The sensory supply to the upper airway
is derived from the cranial nerves ( Figure 19–3). The mucous membranes of the nose
are innervated by the ophthalmic division (V1)
of the trigeminal nerve anteriorly (anterior ethmoidal nerve) and by the
maxillary division (V 2) posteriorly (sphenopala-tine nerves).
The palatine nerves provide sensory fibers from the trigeminal nerve (V) to the
supe-rior and inferior surfaces of the hard and soft pal-ate. The olfactory nerve (cranial nerve I)
innervates the nasal mucosa to provide the sense of smell. The lingual nerve (a
branch of the mandibular division [V3]
of the trigeminal nerve) and the glossopharyn-geal nerve (the ninth cranial
nerve) provide general sensation to the anterior two-thirds and posterior
one-third of the tongue, respectively. Branches of the facial nerve (VII) and
glossopharyngeal nerve provide the sensation of taste to those areas,
respec-tively. The glossopharyngeal
nerve also innervates the roof of the pharynx, the tonsils, and the
under-surface of the soft palate. The vagus
nerve (the tenth cranial nerve) provides sensation to the airway below the
epiglottis. The superior laryngeal branch of the vagus divides into an external
(motor) nerve and an internal (sensory) laryngeal nerve that pro-vide sensory
supply to the larynx between the epi-glottis and the vocal cords. Another
branch of the vagus, the recurrent
laryngeal nerve, innervates the larynx below the vocal cords and the
trachea.
The muscles of the larynx are innervated
by the recurrent laryngeal nerve, with the exception of the cricothyroid
muscle, which is innervated by the exter-nal (motor) laryngeal nerve, a branch
of the superior laryngeal nerve. The posterior cricoarytenoid mus-cles abduct
the vocal cords, whereas the lateral crico-arytenoid muscles are the principal
adductors.
Phonation involves complex simultaneous
actions by several laryngeal muscles. Damage to the motor nerves innervating
the larynx leads
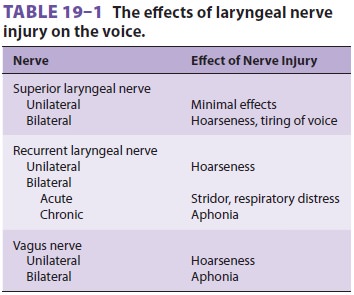
to a spectrum of speech disorders ( Table 19–1).
Unilateral denervation of a cricothyroid muscle causes very subtle clinical
findings. Bilateral palsy of the superior laryngeal nerve may result in hoarse-ness
or easy tiring of the voice, but airway control is not jeopardized.
Unilateral paralysis of a recurrent
laryngeal nerve results in paralysis of the ipsilateral vocal cord, causing
deterioration in voice quality. Assuming intact superior laryngeal nerves, acute bilateral recurrent laryngeal
nerve palsy can result in stri-dor and respiratory distress because of the
remain-ing unopposed tension of the cricothyroid muscles. Airway problems are
less frequent in chronic bilat-eral
recurrent laryngeal nerve loss because of the development of various
compensatory mechanisms (eg, atrophy of the laryngeal musculature).
Bilateral injury to the vagus nerve
affects both the superior and the recurrent laryngeal nerves. Thus, bilateral
vagal denervation produces flaccid, midpositioned vocal cords similar to those
seen after administration of succinylcholine. Although phona-tion is severely
impaired in these patients, airway control is rarely a problem.
The blood supply of the larynx is
derived from branches of the thyroid arteries. The cricothyroid artery arises
from the superior thyroid artery itself, the first branch given off from the
external carotid artery, and crosses the upper cricothyroid membrane (CTM),
which extends from the cricoid cartilage to

the thyroid cartilage. The superior
thyroid artery is found along the lateral edge of the CTM.
The trachea begins beneath the cricoid
cartilage and extends to the carina, the point at which the right and left
main-stem bronchi divide (Figure 19–4). Anteriorly, the trachea consists
of cartilaginous rings; posteriorly, the trachea is membranous.
Related Topics