Chapter: Clinical Anesthesiology: Anesthetic Management: Preoperative Assessment, Premedication, & Perioperative Documentation
Documentation - Clinical Anesthesiology
DOCUMENTATION
Physicians should first and foremost
provide high-quality and efficient medical care. Secondly, they must document
the care that has been provided. Adequate documentation provides guidance to
those who may encounter the patient in the future. It permits others to assess
the quality of the care that was given and to provide risk adjustment of
outcomes. Adequate documentation is required for a physician to submit a bill
for his or her services. Finally, adequate and well-organized documenta-tion
(as opposed to inadequate and sloppy docu-mentation) supports a potential
defense case should a claim for medical malpractice be filed.
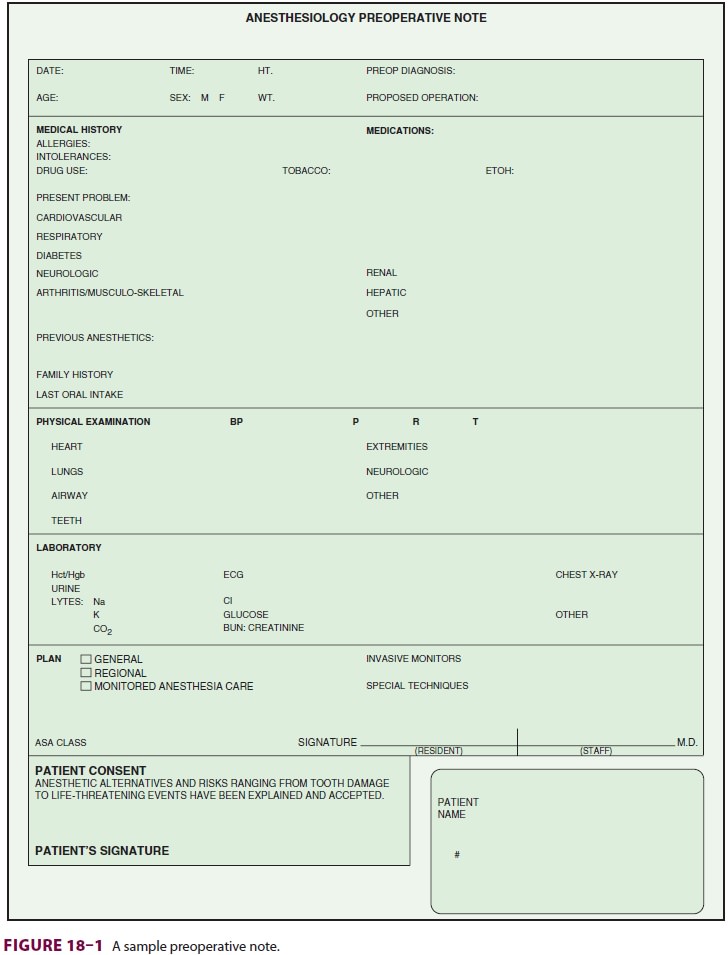
Preoperative Assessment Note
The preoperative assessment note should
appear in the patient’s permanent medical record and should describe pertinent
findings, including the medical history, anesthetic history, current medications
(and whether they were taken on the day of surgery), physical examination, ASA
physical status class, laboratory results, interpretation of imaging,
electro-cardiograms, and recommendations of any consul-tants. A comment is
particularly important when the consultant’s recommendation will not be
followed. As most North American hospitals are transitioning to electronic
medical records, the preanesthetic note will often appear as a standardized
form.
The preoperative note should briefly
describe the anesthetic plan and include a statement regard-ing informed
consent from the patient (or guardian). The plan should indicate whether
regional or general anesthesia (or sedation) will be used, and whether invasive
monitoring or other advanced techniques will be employed. Documentation of the
informed consent discussion sometimes takes the form of a narrative indicating
that the plan, alternative plans, and their advantages and disadvantages
(including their relative risks) were presented, understood, and accepted by
the patient. Alternatively, the patient may be asked to sign a special
anesthesia consent form that contains the same information. A sample
pre-anesthetic report form is illustrated in Figure 18–1.
In the United States, The Joint
Commission (TJC) requires an immediate preanesthetic reevalu-ation to determine
whether the patient’s status has changed in the time since the preoperative
evalu-ation was performed. Even when the elapsed time is less than a minute,
the bureaucracy will not be denied: the “box” must be checked to indicate that
there has been no interval change.
Intraoperative Anesthesia Record
The intraoperative anesthesia record (Figure 18–2)
serves many purposes. It functions as documenta-tion of intraoperative
monitoring, a reference for future anesthetics for that patient, and a source
of data for quality assurance. This record should be terse, pertinent, and
accurate. Increasingly, parts of the anesthesia record are generated
automati-cally and recorded electronically. Such anesthe-sia information
management systems (commonly abbreviated AIMS) have many theoretical and
practical advantages over the traditional paper record but also introduce all
the common pitfalls of
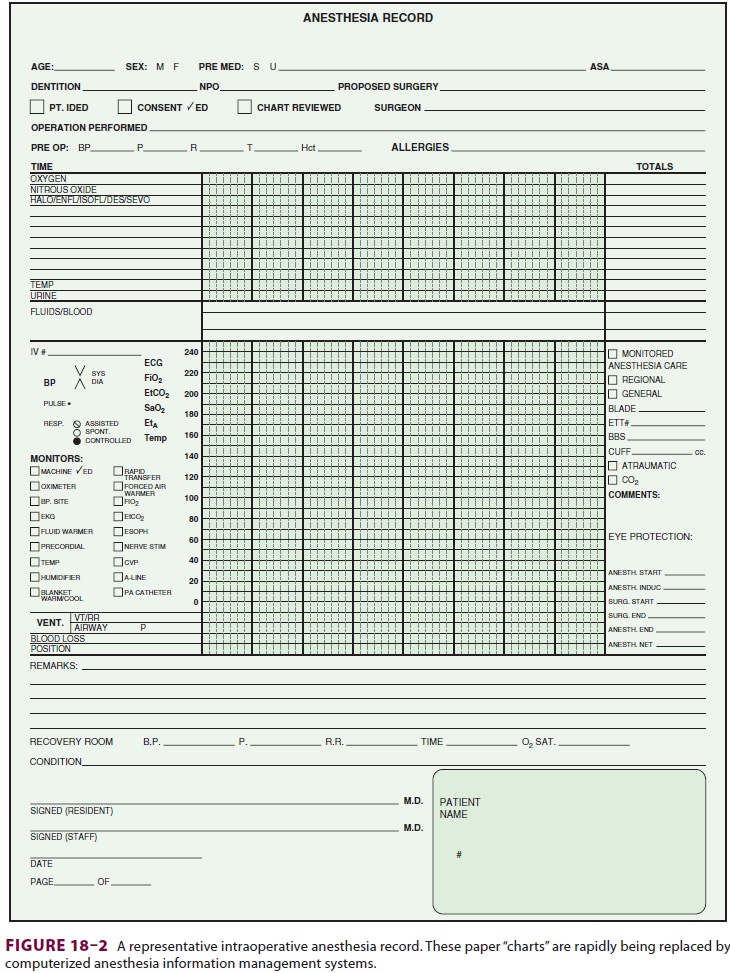
computerization, including the potential
for unrec-ognized recording of artifactual data, the possibility that
practitioners will find attending to the com-puter more interesting than
attending to the patient, and the inevitable occurrence of device and software
shutdowns. Regardless of whether the record is on paper or electronic it should
document the anes-thetic care in the operating room by including the following
elements:
Whether
there has been a preoperative check of the anesthesia machine and other
relevant equipment.
·
Whether
there has been a reevaluation of the patient immediately prior to induction of
anesthesia (a TJC requirement); this generally includes a review of the medical
record to search for any new laboratory results or consultation reports.
·
Time
of administration, dosage, and route of drugs given intraoperatively.
·
Intraoperative
estimates of blood loss and urinary output.
·
Results
of laboratory tests obtained during the operation.
·
Intravenous
fluids and any blood products administered.
·
Pertinent
procedure notes (such as for tracheal intubation or insertion of invasive
monitors).
·
A
notation regarding specialized intraoperative techniques such as the mode of
ventilation, or special techniques such as the use of hypotensive anesthesia,
one-lung ventilation, high-frequency jet ventilation, or cardiopulmonary
bypass.
·
Timing
and conduct of intraoperative events such as induction, positioning, surgical
incision, and extubation.
·
Unusual
events or complications (eg, arrhythmias).
·
Condition
of the patient at the time of release to the postanesthesia or intensive care
unit nurse.
By tradition and convention (and, in the
United States, according to practice guidelines) arterialblood pressure and
heart rate are recorded graphi-cally no less frequently than at 5-min
intervals. Data from other monitors are also usually entered graphi-cally,
whereas descriptions of techniques or compli-cations are described in text. In
some anesthetizing locations of most hospitals the computerized AIMS will be
unavailable. Unfortunately, the conventional, handwritten intraoperative
anesthetic record often proves inadequate for documenting critical inci-dents,
such as a cardiac arrest. In such cases, a sepa-rate text note inserted in the
patient’s medical record may be necessary. Careful recording of the timing of
events is needed to avoid discrepancies between multiple simultaneous records
(anesthesia record, nurses’ notes, cardiopulmonary resuscitation record, and
other physicians’ entries in the medical record). Such discrepancies are
frequently targeted by mal-practice attorneys as evidence of
incompetence,inaccuracy, or deceit. Incomplete, inaccurate, or illegible
records unnecessarily complicatedefending a physician against otherwise
unjustified allegations of malpractice.
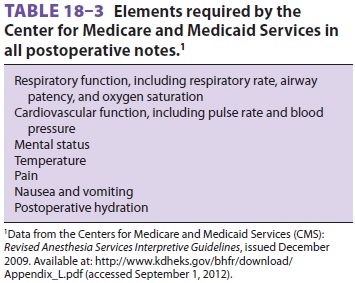
Postoperative Notes
The anesthesiologist’s immediate
responsibility to the patient does not end until the patient has recov-ered
from the effects of the anesthetic. After accom-panying the patient to the
postanesthesia care unit (PACU), the anesthesiologist should remain with the
patient until normal vital signs have been measured and the patient’s condition
is deemed stable. Before discharge from the PACU, a note should be written by
the anesthesiologist to document the patient’s recovery from anesthesia, any
apparent anesthesia-related complications, the immediate postoperative
condition of the patient, and the patient’s disposition (discharge to an
outpatient area, an inpatient ward, an intensive care unit, or home). In the
United States, as of 2009, the Centers for Medicare and Medicaid Services
require that certain elements be included in all postoperative notes ( Table 18–3).
Recovery from anesthesia should be assessed at least once within 48 h after
discharge from the PACU in all inpatients. Postoperative notes should document
the general condition of the patient, the presence or absence of any
anesthesia-related complications, and any mea-sures undertaken to treat such
complications.
Related Topics