Chapter: Clinical Anesthesiology: Anesthetic Management: Airway Management
Complications of Laryngoscopy & Intubation
COMPLICATIONS OF LARYNGOSCOPY & INTUBATION
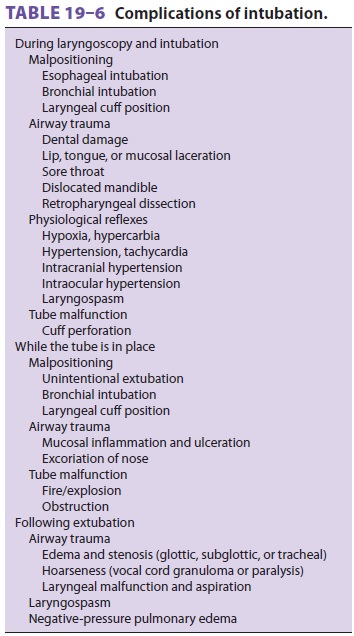
The complications of laryngoscopy and
intuba-tion include hypoxia, hypercarbia, dental and air-way trauma, tube
malpositioning, physiological responses to airway instrumentation, or tube
mal-function. These complications can occur during laryngoscopy and intubation,
while the tube is in place, or following extubation ( Table 19–6).
Airway Trauma
Instrumentation with a metal laryngoscope blade and insertion of a stiff TT often traumatizes delicate airway tissues. Tooth damage is a common cause of (relatively small) malpractice claims against anes-thesiologists. Laryngoscopy and intubation can lead to a range of complications from sore throat to tra-cheal stenosis. Most of these are due to prolonged external pressure on sensitive airway structures. When these pressures exceed the capillary–arteriolar blood pressure (approximately 30 mm Hg), tissue ischemia can lead to a sequence of inflammation, ulceration, granulation, and stenosis. Inflation of a TT cuff to the minimum pressure that creates a seal during routine positive-pressure ventilation (usually at least 20 mm Hg) reduces tracheal blood flow by 75% at the cuff site. Further cuff inflation or induced hypotension can totally eliminate mucosal blood flow.
Postintubation croup caused by glottic,
laryn-geal, or tracheal edema is particularly serious in children. The efficacy
of corticosteroids (eg, dexamethasone—0.2 mg/kg, up to a maximum of 12 mg) in
preventing postextubation airway edema remains controversial; however,
corticosteroids have been demonstrated to be efficacious in children with croup
from other causes. Vocal cord paralysis from cuff compression or other trauma
to the recurrent laryngeal nerve results in hoarseness and increases the risk
of aspiration. The incidence of postopera-tive hoarseness seems to increase
with obesity, dif-ficult intubations, and anesthetics of long duration.
Curiously, applying a water-soluble lubricant or a local anesthetic-containing
gel to the tip or cuff of the does not decrease the incidence of postoperative
sore throat or hoarseness, and, in some studies, actu-ally increased the
incidence of these complications. Smaller tubes (size 6.5 in women and size 7.0
in men) are associated with fewer complaints of postoperative sore throat.
Repeated attempts at laryngoscopy during a difficult intubation may lead to
periglottic edema and the inability to ventilate with a face mask, thus turning
a bad situation into a life-threatening one.
Errors of Tracheal Tube Positioning
Unrecognized esophageal intubation can
pro-duce catastrophic results. Prevention of thiscomplication depends on direct
visualization of the tip of the TT passing through the vocal cords, care-ful
auscultation for the presence of bilateral breath sounds and the absence of
gastric gurgling while ventilating through the TT, analysis of exhaled gas for
the presence of CO2 (the most reliable automated method),
chest radiography, or the use of an FOB.
Even though it is confirmed that the
tube is in the trachea, it may not be correctly positioned. Overly “deep”
insertion usually results in intubation of the right (rather than left)
main-stem bronchus because of the right bronchus’ less acute angle with the
trachea. Clues to the diagnosis of bronchial intubation include unilateral
breath sounds,unexpected hypoxia with pulse oximetry (unreliable with high
inspired oxygen concentrations), inability to palpate the TT cuff in the
sternal notch during cuff inflation, and decreased breathing-bag compli-ance
(high peak inspiratory pressures).
In contrast, inadequate insertion depth
will position the cuff in the larynx, predisposing the patient to laryngeal
trauma. Inadequate depth of insertion can be detected by palpating the cuff
over the thyroid cartilage.
Because no one technique protects
against all possibilities for misplacing a TT, minimal testing should include
chest auscultation, routine capnog-raphy, and occasionally cuff palpation.
If the patient is repositioned, tube
placement must be reconfirmed. Neck extension or lateral rota-tion most often
moves a TT away from the carina, whereas neck flexion most often moves the tube
toward the carina.
At no time should excessive force be
employed during intubation. Esophageal intubations can result in esophageal
rupture and mediastinitis. Mediastinitis presents as severe sore throat, fever,
sepsis, and subcutaneous air often manifesting as crepitus. Early intervention
is necessary to avoid mortality. If esophageal perforation is suspected,
consultation with an otolaryngologist or thoracic surgeon is recommended.
Physiological Responses to Airway Instrumentation
Laryngoscopy and tracheal intubation
violate the patient’s protective airway reflexes and predictably lead to
hypertension and tachycardia when per-formed under “light” planes of general
anesthesia. The insertion of an LMA is typically associated with less
hemodynamic change. Hemodynamic changes can be attenuated by intravenous
admin-istration of lidocaine, opioids, or β-blockers or deeper planes of inhalation
anesthesia in the min-utes before laryngoscopy. Hypotensive agents, including
sodium nitroprusside, nitroglycerin, esmolol and nicardipine, have also been
shown to effectively attenuate the transient hypertensive response associated
with laryngoscopy and intuba-tion. Cardiac arrhythmias—particularly
ventricu-lar bigeminy—sometimes occur during intubation and may indicate light
anesthesia.
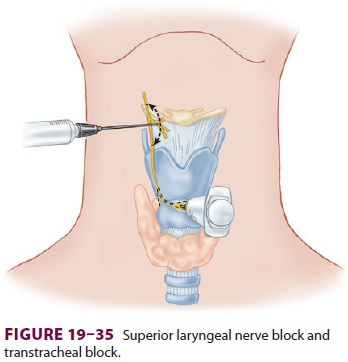
Laryngospasm
is a forceful
involuntary spasmof the laryngeal musculature caused by sensory stimulation of
the superior laryngeal nerve. Triggering stimuli include pharyngeal secretions
or passing a TT through the larynx during extuba-tion. Laryngospasm is usually
prevented by extu-bating patients either deeply asleep or fully awake, but it
can occur—albeit rarely—in an awake patient. Treatment of laryngospasm includes
pro-viding gentle positive-pressure ventilation with an anesthesia bag and mask
using 100% oxygen or administering intravenous lidocaine (1–1.5 mg/kg). If
laryngospasm persists and hypoxia develops, small doses of succinylcholine
(0.25–0.5 mg/kg) may be required (perhaps in combination with small doses of
propofol or another anesthetic) to relax the laryngeal muscles and to allow
controlled ventilation. The large negative intrathoracic pressures generated by
a struggling patientduring laryngospasm can result in the develop-ment of
negative-pressure pulmonary edema, even in healthy patients.
Whereas laryngospasm may result from an
abnormally sensitive reflex, aspiration can result from depression of laryngeal
reflexes following pro-longed intubation and general anesthesia.
Bronchospasm is another reflex response
to intubation and is most common in asthmatic patients. Bronchospasm can
sometimes be a clue to bronchial intubation. Other pathophysiological effects
of intubation include increased intracranial and intraocular pressures.
Tracheal Tube Malfunction
TTs do not always function as intended.
Polyvinyl chloride tubes may be ignited by cautery or laser in an
oxygen/nitrous oxide-enriched environment. Valve or cuff damage is not unusual
and should be excluded prior to insertion. TT obstruction can result from
kinking, from foreign body aspira-tion, or from thick or inspissated secretions
in the lumen.


Related Topics