Chapter: Clinical Anesthesiology: Anesthetic Management: Airway Management
Techniques of Direct and Indirect Laryngoscopy & Intubation
TECHNIQUES OF DIRECT AND INDIRECT LARYNGOSCOPY & INTUBATION
Indications for Intubation
Inserting a tube into the trachea has
become a routine part of delivering a general anesthetic. Intubation is not a
risk-free procedure, and not all patients receiv-ing general anesthesia require
it. A TT is generally placed to protect the airway and for airway access.
Intubation is indicated in patients who are at risk of aspiration and in those
undergoing surgical proce-dures involving body cavities or the head and neck.
Mask ventilation or ventilation with an LMA is usu-ally satisfactory for short
minor procedures such as cystoscopy, examination under anesthesia, inguinal
hernia repairs, extremity surgery, and so forth.
Preparation for Direct Laryngoscopy
Preparation for intubation includes
checking equip-ment and properly positioning the patient. The TT should be
examined. The tube’s cuff inflation system can be tested by inflating the cuff
using a 10-mL syringe. Maintenance of cuff pressure after detachingthe syringe ensures proper cuff and valve
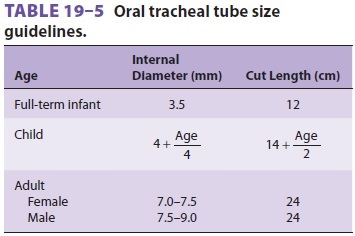
function.Some anesthesiologists cut the TT to a preset length to decrease the
dead space, the risk of bronchial intubation, and the risk of occlusion from
tube kink-ing (Table 19–5). The connector should be pushed firmly into the tube
to decrease the likelihood of dis-connection. If a stylet is used, it should be
inserted
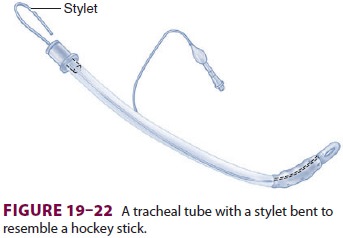
into the TT, which is then bent to resemble a hockey stick (Figure 19–22). This shape facilitates intuba-tion of an anteriorly positioned larynx. The desired blade is locked onto the laryngoscope handle, and bulb function is tested. The light intensity should remain constant even if the bulb is jiggled. A blink-ing light signals a poor electrical contact, whereas fading indicates depleted batteries. An extra handle, blade, TT (one size smaller than the anticipated optimal size), and stylet should be immediately available. A functioning suction unit is needed to clear the airway in case of unexpected secretions, blood, or emesis.
Successful intubation often depends on correct
patient positioning. The patient’s head should be level with the
anesthesiologist’s waist or higher to prevent unnecessary back strain during
laryngoscopy.
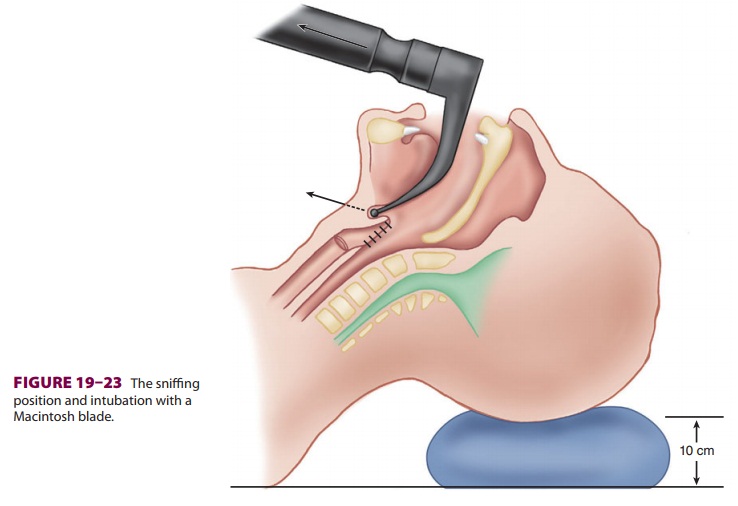
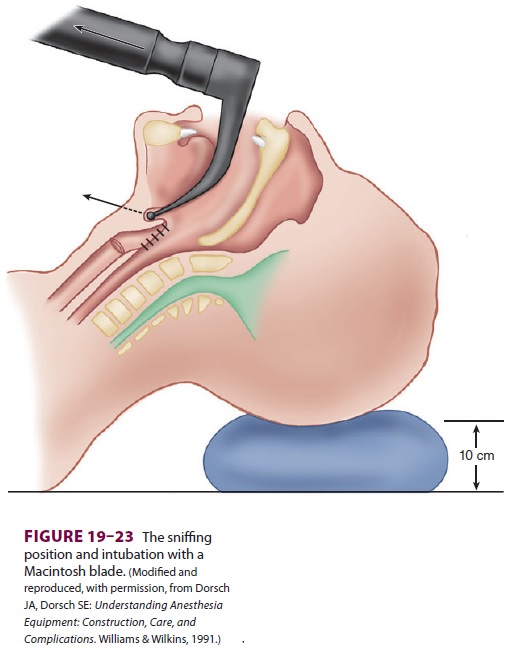
Direct laryngoscopy displaces pharyngeal
soft tissues to create a direct line of vision from the mouth to the glottic
opening. Moderate head eleva-tion (5–10 cm above the surgical table) and
exten-sion of the atlantooccipital joint place the patient in the desired
sniffing position (Figure 19–23). The lower portion of the
cervical spine is flexed by rest-ing the head on a pillow or other soft
support.
Preparation for induction and intubation
also involves routine preoxygenation. Administration of 100% oxygen provides an
extra margin of safety in
case the patient is not easily
ventilated after induc-tion. Preoxygenation can be omitted in patients who
object to the face mask; however, failing to preoxy-genate increases the risk
of rapid desaturation fol-lowing apnea.
Because general anesthesia abolishes the
pro-tective corneal reflex, care must be taken during this period not to injure
the patient’s eyes by uninten-tionally abrading the cornea. Thus, the eyes are
rou-tinely taped shut, often after applying an ophthalmic ointment before
manipulation of the airway.
Orotracheal Intubation
The laryngoscope is held in the left
hand. With the patient’s mouth opened the blade is introduced into the right
side of the oropharynx—with care to avoid the teeth. The tongue is swept to the
left and up into the floor of the pharynx by the blade’s flange. Successful
sweeping of the tongue leftward clears the view for TT placement. The tip of a
curved blade is usually inserted into the vallecula, and the straight blade tip
covers the epiglottis. With either blade, the handle is raised up and away from
the patient in a plane perpendicular to the patient’s mandible to expose the
vocal cords (Figure
19–24). Trapping a lip between the teeth and the blade and leverage
on the teeth are avoided. The TT is taken with the right hand, and its tip is
passed through the abducted vocal cords. The “backward, upward, rightward,
pressure” (BURP) maneuver applied externally moves an anteriorly positioned
glottis posterior to facilitate visualiza-tion of the glottis. The TT cuff
should lie in the upper trachea, but beyond the larynx. The laryngo-scope is
withdrawn, again with care to avoid tooth damage. The cuff is inflated with the
least amount of air necessary to create a seal during positive-pressure
ventilation to minimize the
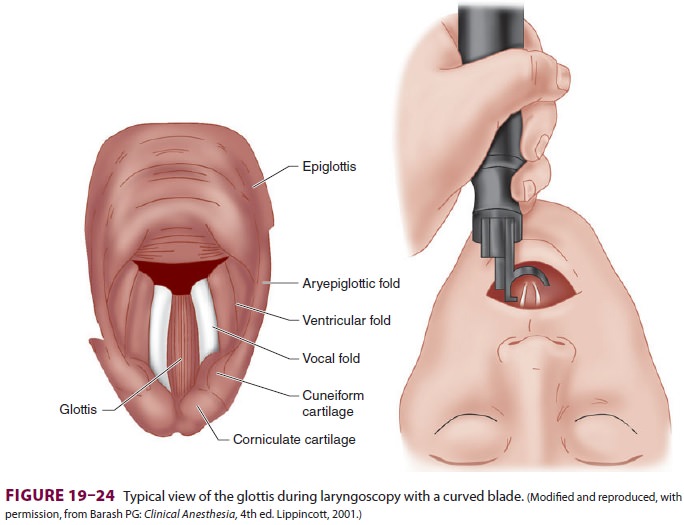
pressure transmitted to the tracheal
mucosa. Overinflation beyond 30 mm Hg may inhibit capil-lary blood flow,
injuring the trachea. Compressing the pilot balloon with the fingers is not a reliable method of determining
whether cuff pressure is either sufficient or excessive.
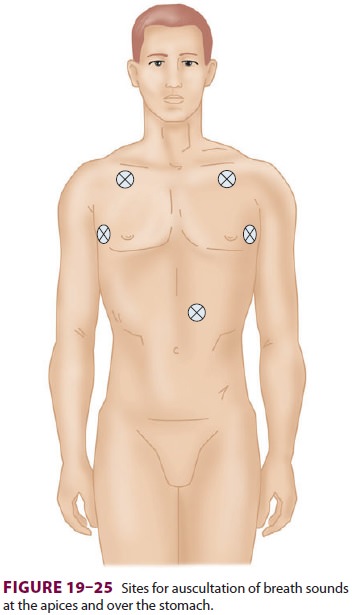
After intubation, the chest and
epigastrium are immediately auscultated, and a capnographic trac-ing (the
definitive test) is monitored to ensure intratracheal location ( Figure 19–25).
If there is doubt as to whether the tube is in the esophagus or trachea, repeat
the laryngoscopy to confirm place-ment. End-tidal CO 2 will not be produced if there is no cardiac output.
FOB through the tube and visualization of the tracheal rings and carina will
likewise confirm correct placement. Otherwise, the tube is taped or tied to
secure its position.Although the persistent detection of CO2 by a
capnograph is the best confirmation of tracheal placement of a TT, it cannot
exclude bron-chial intubation. The earliest evidence of bronchial intubation
often is an increase in peak inspiratory pressure. Proper tube location can be
reconfirmed by palpating the cuff in the sternal notch while compressing the
pilot balloon with the other hand.The cuff should not be felt above the level
of the cricoid cartilage, because a prolongedintralaryngeal location may result
in postoperative hoarseness and increases the risk of accidental extubation.
Tube position can also be documented by chest radiography.
The description presented here assumes
an unconscious patient. Oral intubation is usually poorly tolerated by awake,
fit patients. Intravenous sedation, application of a local anesthetic spray in
the oropharynx, regional nerve block, and constant reassurance will improve
patient acceptance.
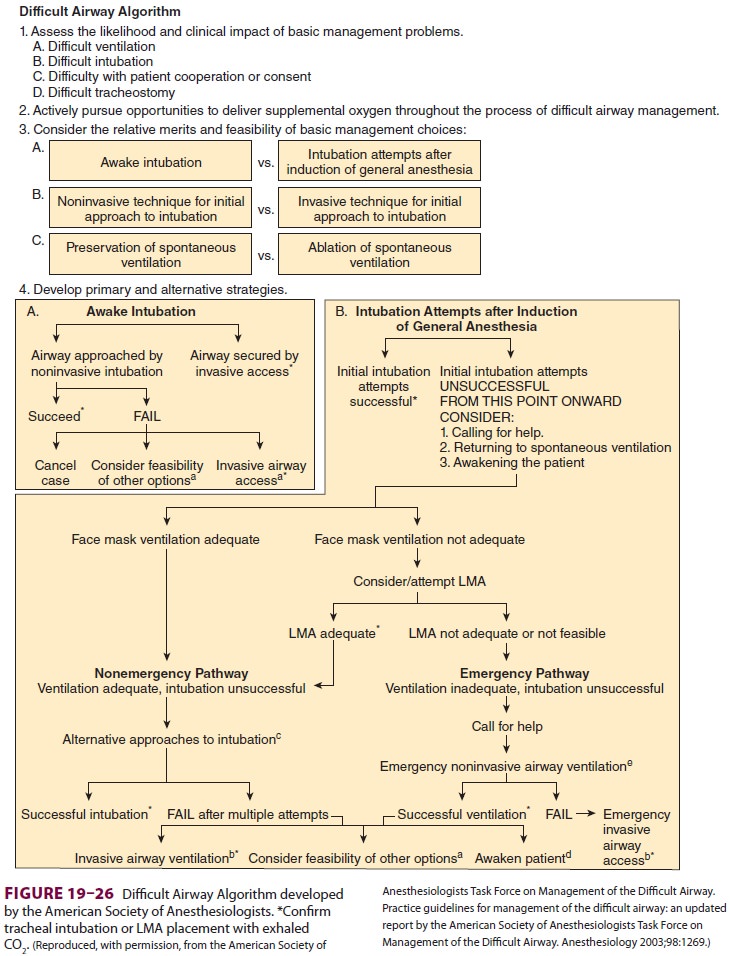
A failed intubation should not be
followed by identical repeated attempts. Changes must be made to increase the
likelihood of success, such as repositioning the patient, decreasing the tube
size, adding a stylet, selecting a different blade, using an indirect
laryngoscope, attempting a nasal route, or requesting the assistance of another
anesthesiolo-gist. If the patient is also difficult to ventilate with a mask,
alternative forms of airway management (eg, LMA, Combitube, cricothyrotomy with
jet ven-tilation, tracheostomy) must be immediately pur-sued. The guidelines
developed by the American Society of Anesthesiologists for the management of a
difficult airway include a treatment plan algorithm (Figure 19–26).
Use of video or indirect laryngoscopes
is dependent upon the design of the device. Some devices are placed midline
without the requirement to sweep the tongue from view. Other devices con-tain
channels to direct the endotracheal tube to the glottic opening. Practitioners
should be familiar with the features of available devices well in advance of
using one in a difficult airway situation. The com-bined use of a video
laryngoscope and an intubation
Difficult Airway Algorithm
Assess the likelihood and
clinical impact of basic management problems.
Difficult ventilation
Difficult intubation
Difficulty with patient
cooperation or consent
Difficult tracheostomy
Actively pursue
opportunities to deliver supplemental oxygen throughout the process of
difficult airway management.
Consider the relative merits and feasibility of basic management
choices:
bougie often can facilitate intubation,
when the endotracheal tube cannot be directed into the glot-tis despite good
visualization of the laryngeal open-ing (Figure 19–27).
Nasotracheal Intubation
Nasal intubation is similar to oral
intubation except that the TT is advanced through the nose and naso-pharynx
into the oropharynx before laryngoscopy. The nostril through which the patient
breathes most easily is selected in advance and prepared. Phenylephrine nose
drops (0.5% or 0.25%) vaso-constrict vessels and shrink mucous membranes. If
the patient is awake, local anesthetic ointment (for the nostril), spray (for
the oropharynx), and nerve blocks can also be utilized.
A TT lubricated with water-soluble jelly
is introduced along the floor of the nose, below the inferior turbinate, at an angle perpendicular tothe face.
The tube’s bevel should be directed later-ally away from the turbinates. To
ensure that the tube passes along the floor of the nasal cavity, the proximal
end of the TT should be pulled cephalad. The tube is gradually advanced, until
its tip can be visualized in the oropharynx. Laryngoscopy, as dis-cussed, reveals
the abducted vocal cords. Often the distal end of the TT can be pushed into the
trachea without difficulty. If difficulty is encountered, the tip of the tube
may be directed through the vocal cords with Magill forceps, being careful not
to damage the cuff. Nasal passage of TTs, airways, or nasogastric catheters
carries greater risk in patients with severe mid-facial trauma because of the
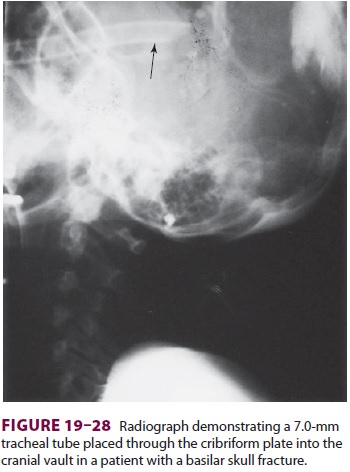
risk of intracranial placement (Figure 19–28).
Although less used today, blind nasal
intuba-tion of spontaneously breathing patients can be employed. In this
technique, after applying topi-cal anesthetic to the nostril and pharynx, a
breath-ing tube is passed through the nasopharynx. Using
breath sounds as a guide, it is directed
toward the glottis. When breath sounds are maximal, the anes-thetist advances
the tube during inspiration in an effort to blindly pass the tube into the
trachea.
Flexible Fiberoptic Intubation
Fiberoptic intubation (FOI) is routinely
performed in awake or sedated patients with problematic air-ways. FOI is ideal
for:
·
A
small mouth opening
·
Minimizing
cervical spine movement in trauma or rheumatoid arthritis
·
Upper
airway obstruction, such as angioedema or tumor mass
·
Facial
deformities, facial trauma
·
FOI
can be performed awake or asleep via oral or nasal routes.
·
Awake
FOI: predicted inability to ventilate by mask, upper airway obstruction
·
Asleep
FOI: Failed intubation, desire for minimal C spine movement in patients who
refuse awake intubation
·
Oral
FOI: Facial, skull injuries
·
Nasal
FOI: A poor mouth opening
When FOI is considered, careful planning
is necessary, as it will likely add to the anesthesia time prior to surgery.
Patients should be informed of the need for awake intubation as a part of the
informed consent process.
The airway is anesthetized with a local
anes-thetic spray, and patient sedation is provided, as tolerated.
Dexmedetomidine has the advantage of preserving respiration while providing
seda-tion. Airway anesthesia is discussed in the Case Discussion below.
If nasal FOI is planned, both nostrils
are pre-pared with vasoconstrictive drops. The nostril through which the
patient breathes more easily is identified. Oxygen can be insufflated through
the suction port and down the aspiration channel of the FOB to improve
oxygenation and blow secretions away from the tip.
Alternatively, a large nasal airway (eg,
36F) can be inserted in the contralateral nostril. The breath-ing circuit can
be directly connected to the end of this nasal airway to administer 100% oxygen
during laryngoscopy. If the patient is unconscious and not breathing
spontaneously, the mouth can be closed and ventilation attempted through the
single nasal airway. When this technique is used, adequacy of ventilation and
oxygenation should be confirmed by capnography and pulse oximetry. The
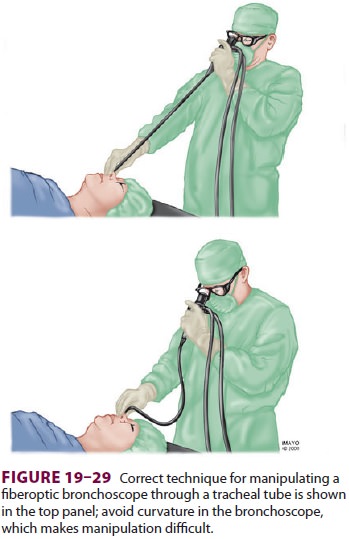
lubricated shaft of the FOB is introduced into the TT lumen. It is important to
keep the shaft of the broncho-scope relatively straight (Figure 19–29) so that if the
head of the bronchoscope is rotated in one direction, the distal end will move
to a similar degree and in the same direction. As the tip of the FOB passes
through the distal end of the TT, the epiglottis or glottis should be visible.
The tip of the bronchoscope is manipulated, as needed, to pass the abducted
cords.
Having an assistant thrust the jaw
forward or apply cricoid pressure may improve visualiza-tion in difficult
cases. If the patient is breathing
spontaneously, grasping the tongue with
gauze and pulling it forward may also facilitate intubation.
Once in the trachea, the FOB is advanced
to within sight of the carina. The presence of tracheal rings and the carina is
proof of proper position-ing. The TT is pushed off the FOB. The acute angle
around the arytenoid cartilage and epiglottis may prevent easy advancement of
the tube. Use of an armored tube usually decreases this problem due to its
greater lateral flexibility and more obtusely angled distal end. Proper TT
position is confirmed by viewing the tip of the tube an appropriate dis-tance
(3 cm in adults) above the carina before the FOB is withdrawn.
Oral FOI proceeds similarly, with the aid of various oral airway devices to direct the FOB toward the glottis and to reduce obstruction of the view by the tongue.
Related Topics