Chapter: Medical Physiology: Parathyroid Hormone, Calcitonin, Calcium and Phosphate Metabolism, Vitamin D, Bone, and Teeth
Vitamin D and Actions of Vitamin D
Vitamin D
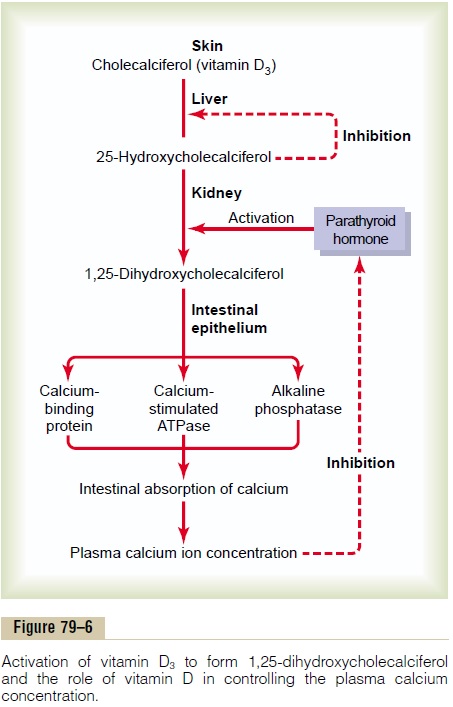
Vitamin D has a potent effect to increase calcium absorption from the intestinal tract; it also has impor-tant effects on both bone deposition and bone absorption, as discussed later. However, vitamin D itself is not the active substance that actually causes these effects. Instead, vitamin D must first be converted through a succession of reactions in the liver and the kidneys to the final active product, 1,25-dihydroxycholecalciferol, also called 1,25(OH)2D3. Figure 79–6 shows the suc-cession of steps that lead to the formation of this sub-stance from vitamin D. Let us discuss these steps.
Cholecalciferol (Vitamin D3) Is Formed in the Skin. Severalcompounds derived from sterols belong to the vitamin D family, and they all perform more or less the same functions. Vitamin D3 (also called cholecalciferol) is the most important of these and is formed in the skin as a result of irradiation of 7-dehydrocholesterol, a sub-stance normally in the skin, by ultraviolet rays from the sun. Consequently, appropriate exposure to the sun prevents vitamin D deficiency. The additional vitamin D compounds that we ingest in food are iden-tical to the cholecalciferol formed in the skin, except for the substitution of one or more atoms that do not affect their function.
Cholecalciferol Is Converted to 25-Hydroxycholecalciferol in the Liver. The first step in the activation of cholecal-ciferol is to convert it to 25-hydroxycholecalciferol; this occurs in the liver. The process is a limited one, because the 25-hydroxycholecalciferol has a feedback inhibitory effect on the conversion reactions. This feedback effect is extremely important for two reasons.
First, the feedback mechanism precisely regulates the concentration of 25-hydroxycholecalciferol in the plasma, an effect that is shown in Figure 79–7. Note that the intake of vitamin D3 can increase many times,

and yet the concentration of 25-hydroxycholecalcif-erol remains nearly normal. This high degree of feed-back control prevents excessive action of vitamin D when intake of vitamin D3 is altered over a wide range.
Second, this controlled conversion of vitamin D3 to 25-hydroxycholecalciferol conserves the vitamin D stored in the liver for future use. Once it is converted, it persists in the body for only a few weeks, whereas in the vitamin D form, it can be stored in the liver for many months.
Formation of 1,25-Dihydroxycholecalciferol in the Kidneys and Its Control by Parathyroid Hormone. Figure 79–6also shows the conversion in the proximal tubules of the kidneys of 25-hydroxycholecalciferol to 1,25-dihydroxycholecalciferol. This latter substance is by farthe most active form of vitamin D, because the previ-ous products in the scheme of Figure 79–6 have less than 1/1000 of the vitamin D effect. Therefore, in the absence of the kidneys, vitamin D loses almost all its effectiveness.
Note also in Figure 79–6 that the conversion of 25-hydroxycholecalciferol to 1,25-dihydroxycholecalcif-erol requires PTH. In the absence of PTH, almost none of the 1,25-dihydroxycholecalciferol is formed. Therefore, PTH exerts a potent influence in determin-ing the functional effects of vitamin D in the body.
Calcium Ion Concentration Controls the Formation of 1,25-Dihydroxycholecalciferol. Figure 79–8 demonstrates thatthe plasma concentration of 1,25-dihydroxycholecal-ciferol is inversely affected by the concentration of calcium in the plasma. There are two reasons for this. First, the calcium ion itself has a slight effect in pre-venting the conversion of 25-hydroxycholecalciferol to 1,25-dihydroxycholecalciferol. Second, and even more important, as we shall see later, the rate of secretion of PTH is greatly suppressed when the plasma calcium ion concentration rises above 9 to 10 mg/100 ml. Therefore, at calcium concentrations below this level, PTH promotes the conversion of 25-hydroxycholecalciferol to 1,25-dihydroxycholecalcif-erol in the kidneys. At higher calcium concentrations, when PTH is suppressed, the 25-hydroxycholecalcif-erol is converted to a different compound—24,25-dihydroxycholecalciferol—that has almost no vitamin D effect.
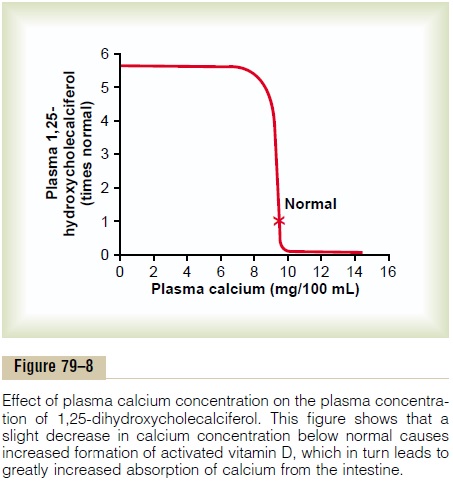
When the plasma calcium concentration is already too high, the formation of 1,25-dihydroxycholecalcif-erol is greatly depressed. Lack of this in turn decreases the absorption of calcium from the intestines, the bones, and the renal tubules, thus causing the calcium ion concentration to fall back toward its normal level.
Actions of Vitamin D
The active form of vitamin D, 1,25-dihydroxycholecal-ciferol, has several effects on the intestines, kidneys, and bones that increase absorption of calcium and phosphate into the extracellular fluid and contribute to feedback regulation of these substances.
“Hormonal” Effect of Vitamin D to Promote Intestinal Calcium Absorption. 1,25-Dihydroxycholecalciferol itself func-tions as a type of “hormone” to promote intestinal absorption of calcium. It does this principally by increasing, over a period of about 2 days, formation of a calcium-binding protein in the intestinal epithelial cells. This protein functions in the brush border of these cells to transport calcium into the cell cytoplasm, and the calcium then moves through the basolateral membrane of the cell by facilitated diffusion. The rate of calcium absorption is directly proportional to the quantity of this calcium-binding protein. Furthermore, this protein remains in the cells for several weeks after the 1,25-dihydroxycholecalciferol has been removed from the body, thus causing a prolonged effect on calcium absorption.
Other effects of 1,25-dihydroxycholecalciferol that might play a role in promoting calcium absorption are the formation of (1) a calcium-stimulated ATPase in the brush border of the epithelial cells and (2) an alka-line phosphatase in the epithelial cells. The precise details of all these effects are unclear.
Vitamin D Promotes Phosphate Absorption by the Intestines.
Although phosphate is usually absorbed easily, phos-phate flux through the gastrointestinal epithelium is enhanced by vitamin D. It is believed that this results from a direct effect of 1,25-dihydroxycholecalciferol, but it is possible that it results secondarily from this hormone’s action on calcium absorption, the cal-cium in turn acting as a transport mediator for the phosphate.
Vitamin D Decreases Renal Calcium and Phosphate Excretion.
Vitamin D also increases calcium and phosphate absorption by the epithelial cells of the renal tubules, thereby tending to decrease excretion of these sub-stances in the urine. However, this is a weak effect and probably not of major importance in regulating the extracellular fluid concentration of these substances.
Effect of Vitamin D on Bone and Its Relation to Parathyroid Hormone Activity. Vitamin D plays important roles inboth bone absorption and bone deposition. The administration of extreme quantities of vitamin Dcauses absorption of bone. In the absence of vitaminD, the effect of PTH in causing bone absorption (dis-cussed in the next section) is greatly reduced or even prevented. The mechanism of this action of vitamin D is not known, but it is believed to result from the effect of 1,25-dihydroxycholecalciferol to increase calcium transport through cellular membranes.
Vitamin D in smaller quantities promotes bone cal-cification. One of the ways in which it does this is toincrease calcium and phosphate absorption from the intestines. However, even in the absence of such increase, it enhances the mineralization of bone. Here again, the mechanism of the effect is unknown, but it probably also results from the ability of 1,25-dihy-droxycholecalciferol to cause transport of calcium ions through cell membranes—but in this instance, perhaps in the opposite direction through the osteoblastic or osteocytic cell membranes.
Related Topics