Chapter: Medicine and surgery: Genitourinary system
Urinary stones
Urinary stones
Urinary stones
Definition
The development of stones in the urinary tract or urolithiasis.
Incidence/prevalence
Affects about 10% of the population at some time in their lives.
Age
Peaks age 20ŌĆō50 years.
Sex
M > F (4:1)
Aetiology
Risk factors include: dehydration, urinary tract infections, disorders of calcium handling (hypercalcaemia, hypercalciuria), hyperuricaemia, small intestinal disease or resection, renal tubular acidosis, hereditary conditions (such as cystinuria) and drugs in particular sulphonamides at high doses and indinavir (a protease inhibitor used to treat HIV).
Pathophysiology
Stone formation usually occurs because compounds of low solubility are present in the urine in high concentrations. There are inorganic inhibitors of crystal formation, such as magnesium, citrate and organic inhibitors such as glycoseaminoglycans and nephrocalcin. Uric acid appears to interfere with this inhibition, so when present in high concentrations it predisposes to the formation of both uric acid and nonuric acid stones.
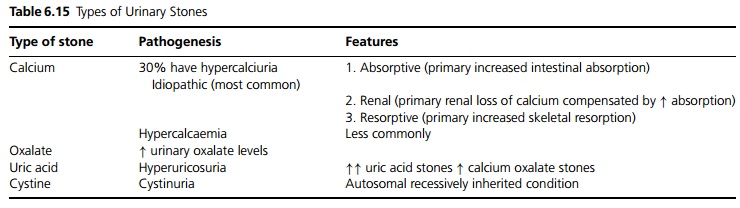
Stones commonly contain calcium oxalate (80%) but about half of these also contain hydroxyapatite. Ōł╝10% are struvite (magnesium ammonium phosphate) stones which consist of struvite and calcium carbonate-apatite), with the remainder formed of calcium phosphate, uric acid or cystine (see Table 6.15).
Clinical features
Renal or ureteric colic is the most common presentation. The pain is characteristically in sharp, intense waves over a background pain, occurring in the loin, radiating to the groin and testes or labia. Patients feel sick and often vomit. They are restless and move around trying to relieve the pain. Bladder or urethral stones may cause pain on passing urine, inability to pass urine or the sensation of passing gravel. Ninety per cent have haematuria, some may have proteinuria.
Infection may present as an acute, recurrent or chronic cystitis, pyelonephritis or pyonephrosis (obstruction with a stone can lead to hydronephrosis, which if this then becomes infected, can make the patient very un-well).
If the stone obstructs a single functioning kidney, postrenal acute renal failure results.
Investigations
Plain AXR: Most stones are radio-opaque and show up on plain abdominal X-rays. Calcium oxalate stones look spiky, calcium phosphate stones are often smooth and can be large. Uric acid stones are radiolucent and cystine stones only slightly radio-opaque.
IVU: i.v. contrast with AXR at 5 and 20 minutes to show exactly where the stone is in relation to the kidneys and ureters. This should be avoided if there is significant renal impairment because excretion is poor so that images are less informative and there is an increased risk of contrast causing acute renal failure.
Renal ultrasound may show stones inside kidney and demonstrate hydronephrosis due to obstruction. CT is often more sensitive.
Serial X-rays to see if stone is moving.
Urine microscopy and culture. Strain all urine to try to catch the stone so that it can be analysed. Crystals may be seen in urine which can help identify the type of stone.
Management
Treat pain, e.g. with opiates and/or NSAID such as diclofenac (useful i.m. or as a suppository). Some recommend anti-spasmodic drugs. Ensure adequate fluid in-take. Stones Ōēź5 mm in diameter are less likely to pass, stones <5 mm especially in the lower half of ureter are more likely to pass without intervention.
Surgical techniques are needed if the stone does not pass. It may be necessary to relieve obstruction urgently, if there is obstruction or infection. Obstruction can be relieved by retrograde stent insertion (usually requires general anaesthetic), or percutaneous nephrostomy insertion under local anaesthetic.
Lithotripsy (external ultrasound shock waves), US guided, no need for anaesthetic. Stones within calyces cannot be broken up this way.
Lasertripsy, electrical.
Open surgery (nephrolithotomy or ureterolithotomy), or percutaneous removal via a nephrostomy. Alternatively perurethral by cystoscopy with a Dormia basket for low stones.
Subsequent management
To reduce the risk of recurrence, all patients should be advised to drink plenty of fluid, especially at night and to treat urinary infections early.
┬Ę Patients with calcium stones should avoid calcium in-take and vitamin D supplements. Potassium citrate may also be given to increase urine levels of citrate which inhibits calcium stone formation.
┬Ę Oxalate is found in tea, chocolate, nuts, strawberries, spinach, rhubarb and beans.
┬Ę Uric acid excretion can be reduced using allopurinol.
┬Ę Cystine stones can be reduced using oral sodium bicarbonate to alkalinise the urine, or D-penicillamine.
Consider looking for predisposing factors such as plasma calcium and parathyroid hormone (if radio-opaque stone), phosphate, urate if radiolucent stones, and 24 hour collection of urine for components of stones.
Prognosis
Despite preventative strategies recurrence rates are as high as 75%.
Related Topics