Chapter: Basic & Clinical Pharmacology : Hypothalamic & Pituitary Hormones
Treatment of Obesity
TREATMENT OF OBESITY
It is said that the developed world is experiencing an “epidemic of obesity.” This statement is based on statistics showing that in the USA, for example, 30–40% of the population is above optimal weight and that the excess weight (especially abdominal fat) is often associated with the metabolic syndrome and increased risks of cardiovascular disease and diabetes. Since eating behav-ior is an expression of endocrine, neurophysiologic, and psycho-logical processes, prevention and treatment of obesity are complex. It is not surprising that there is considerable scientific and financial interest in developing pharmacologic therapy for the condition.
Although obesity can be defined as excess adipose tissue, it is currently quantitated by means of the body mass index (BMI), calculated from BMI = weight (in kilograms)/height2 (in meters). Using this measure, a normal BMI is defined as 18.5–24.9; over-weight, 25–29.9; obese, 30–39.9; and morbidly obese (ie, at very high risk), ≥ 40. Some extremely muscular individuals may have a BMI higher than 25 and no excess fat; however, the BMI scale generally correlates with the degree of obesity and with risk.
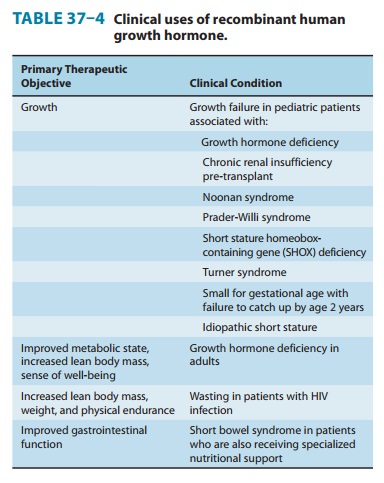
Although the cause of obesity can be simply stated as energy intake (dietary calories) exceeding energy output (resting metab-olism plus exercise), the actual physiology of weight control is extremely complex, and the pathophysiology of obesity is still poorly understood. Many hormones and neuronal mechanisms regulate intake (appetite, satiety), processing (absorption, conver-sion to fat, glycogen, etc), and output (thermogenesis, muscle work). The fact that a large number of hormones reduce appetite (Table 37–4.1, see online version of this book) might appear to offer many targets for weight-reducing drug therapy, but despite intensive research, no available pharmacologic therapy has succeeded in maintaining a weight loss of over 10% for 1 year. Furthermore, the social and psychological aspects of eating are powerful influences that are independent of or only partially dependent on the physiologic control mechanisms. In contrast, bariatric (weight-reducing) surgery readily achieves a sustained weight loss of 10–40%. Furthermore, surgery that bypasses the stomach and upper small intestine (but not simple restrictive banding) rapidly reverses some aspects of the metabolic.
syndrome even before significant weight is lost. However, even a 5–10% loss of weight is associated with a reduction in blood pres-sure and improved glycemic control.
Until approximately 15 years ago, the most popular and successful appetite suppressants were the nonselective 5-HT2 agonists: fenfluramine and dexfenfluramine. Combined with phentermine as Fen-Phen and Dex-Phen, they were moderately effective. However, these drugs were found to cause pulmonary hypertension and cardiac valve defects and were withdrawn.
Older drugs still available in the United States and some other countries include phenylpropanolamine, benzphetamine, amphet-amine, methamphetamine, phentermine, diethylpropion, mazindol, and phendimetrazine. These drugs are all amphetamine mimics and are central nervous system appetite suppressants; they are generally helpful only during the first few weeks of therapy. Their toxicity is significant and includes hypertension (with a risk of cerebral hemor-rhage) and addiction liability.
Orlistat is the only non-amphetamine drug currently approved in the United States for the treatment of obesity. Two other drugs that have been intensely studied are listed in Table 37–5. Clinical trials and phase 4 reports suggest that orlistat is modestly effec-tive for the duration of therapy (up to 1 year) and is probably safer than the amphetamine mimics. However, it does not pro-duce more than a 5–10% loss of weight. Sibutramine was mar-keted for several years but was withdrawn because of increasing evidence of cardiovascular toxicity. Lorcaserin received intense study through 2010 and was submitted for approval to the FDA, but this was denied on the basis of considerations of inadequate safety and effectiveness.
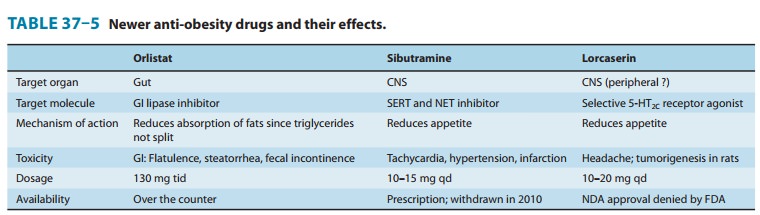
Because of the low efficacy of the drugs listed in Table 37–5, intensive research continues. (Some drugs approved for other indications that reduce appetite and possible future weight loss drugs are set forth in Table 37–5.1, see online version of this book). Because of the redundancy of the physiologic mecha-nisms for control of body weight, it seems likely that polyphar-macy targeting multiple pathways will be needed to achieve success.
Related Topics