Chapter: Biology of Disease: Transfusion and Transplantation
Hemopoietic Stem Cell Transplantation
HEMOPOIETIC STEM CELL TRANSPLANTATION
The transplantation of hemopoietic stem cells is used to correct some immu-nodeficiency diseases and during the treatment for some types of cancer, such as leukemias and lymphomas . Patients with total bone marrow failure, such as in aplastic anemia, or partial failure, as seen in some of the hemoglobinopathies, may also benefit from a stem cell transplant (SCT).
Hemopoietic stem cells for transplantation may be derived from bone mar-row, from peripheral blood, and from umbilical cord blood and SCTs may be autologous, syngeneic or allogeneic. In an autologous transplant the patient’s own stem cells are harvested prior to a treatment in which their own stem cells are destroyed, as, for example, in patients who receive radiation treat-ment or high dose chemotherapy to treat leukemia. The stem cells are stored in liquid nitrogen until the transplant can take place, when they are thawed and reinfused.
A SCT between identical twins is called a syngeneic transplant. In contrast, an allogeneic SCT involves donors and recipients who are genetically nonidenti-cal. The donor could be a sibling or a potential donor identified in a bone mar-row registry (Margin Note 6.4). Donors who are related to the recipient are more likely to be compatible. There is a much greater need for close HLA matching of the donor and recipient involved in bone marrow transplants (BMTs), as GVHD can be a major hazard of this type of transplantation and can occur between seven and 30 days post-transplantation. In the acute form of GVHD epithelial cells in the skin and those lining the intestine are attacked by the sen-sitized T cells originating in the graft. Patients present with a severe maculopa-pular skin rash and sloughing of the intestinal epithelium may lead to diarrhea. Splenomegaly and hepatomegaly occur, as these organs become attacked by T lymphocytes and the patient may become jaundiced. Acute GVHD is fre-quently fatal. A chronic form with similar symptoms may occur over a longer time frame. The patients may suffer frequent secondary infections.
One method of avoiding GVHD is to remove T lymphocytes from SCTs prior to giving the graft. This process, known as T cell depletion involves the use of an antibody to T cells. Once GVHD develops it must be treated with immuno-suppressive drugs
BONE MARROW TRANSPLANTATION
The first successful bone marrow transplant (BMT) was achieved in 1968. Bone marrow contains the hemopoietic stem cells that give rise to all the formed elements of the blood . In bone marrow transplantation (BMT), the donor receives a general or local anesthetic and the marrow is harvested using a needle inserted through the skin over the pelvic bone and into the bone cavity. The process takes approximately one hour to harvest suf-ficient quantity; usually a minimum of 3 q 108 nucleated bone marrow cells containing approximately 2 q 106 stem cells per kilogram of recipient body weight is required. At this stage the marrow may be infused into the recipient or it may require further processing. The marrow is treated to remove blood and plasma, especially if there is a disparity between the ABO blood group of the donor and the recipient. Fragments of bone are removed and the mar-row may also be depleted of T cells to reduce the risk of GVHD prior to intra-venous transfusion into the recipient. The recipient may be given antibiotics because, until the marrow is engrafted and starts to produce blood cells, the patient is at risk of infection. They may also be given platelet and erythrocyte transfusions to prevent bleeding and anemia. A patient receiving a bone mar-row transplant may show adverse side effects, such as nausea, fatigue, hair loss and loss of appetite.
PERIPHERAL BLOOD STEM CELL TRANSPLANTATION
Peripheral blood stem cell transplantation (PBSCT) is the most common form of SCT. Collection of stem cells from peripheral blood is easier both for the collector and the donor. In addition, engraftment of PBSCT is often more rapid than with bone marrow. The donor is treated with granulocyte colony stimulating factor (G-CSF) to increase the number of stem cells in the blood. The stem cells are then obtained from the donor by leukapheresis (MarginNote 6.3). Leukapheresis may take several hours to complete and more thanone session may be needed, with stem cells being stored frozen between donations.
UMBILICAL CORD STEM CELL TRANSPLANTATION
Stem cells may also be obtained from umbilical cord blood, of course with the permission of the family involved. Following birth, blood derived from the baby is obtained from the umbilical cord and the placenta. Since only a small amount of blood is retrieved in this way, the collected stem cells are typically used to treat children.
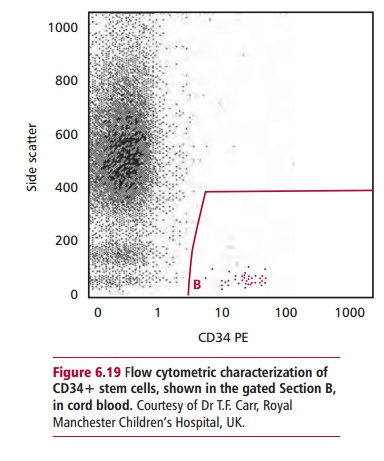
IDENTIFICATION OF HEMOPOIETIC STEM CELLS
Hemopoietic stem cells have a marker protein called CD34 that may be used in their identification. Thus, the numbers of CD34 positive cells in a prepa-ration can be assessed if a sample is stained with a fluorescent antibody to CD34. The cells can be estimated either by using a fluorescence microscope or by flow cytometry . Both peripheral and cord blood may be further processed to obtain the stem cells. For example, an anti-CD34 antibody linked to magnetic particles will bind to CD34+ cells, which can then be purified using a magnet.
Storage of transplant material
Harvested stem cells may be stored for 2–3 days in a refrigerator at 4oC. This may be required, for example, if more than one harvesting procedure is needed or if a patient has to undergo radiation or chemotherapy for cancer treatment prior to receiving the graft. If longer term storage is required, the stem cells may be stored in liquid nitrogen vapour at –176oC. Prior to storage, the cryopreservative dimethylsulfoxide (DMSO) is added to prevent ice crys-tal formation, which would destroy the cells. A programmed freezer allows the cells to be cooled at the optimum rate for cell survival, which is normally approximately 1oC per min.
Post-transplant support
Patients who have just undergone BMT or PBSCT transplantation are highly susceptible to infections. If transfusions of blood products are required, for example for anemia, these products should be free of CMV, a virus which is a latent infection in some individuals. In an immunosuppressed individual, CMV can cause serious illness.
Related Topics