Chapter: Essential Anesthesia From Science to Practice : Applied physiology and pharmacology : A brief pharmacology related to anesthesia
Drugs to raise blood pressure
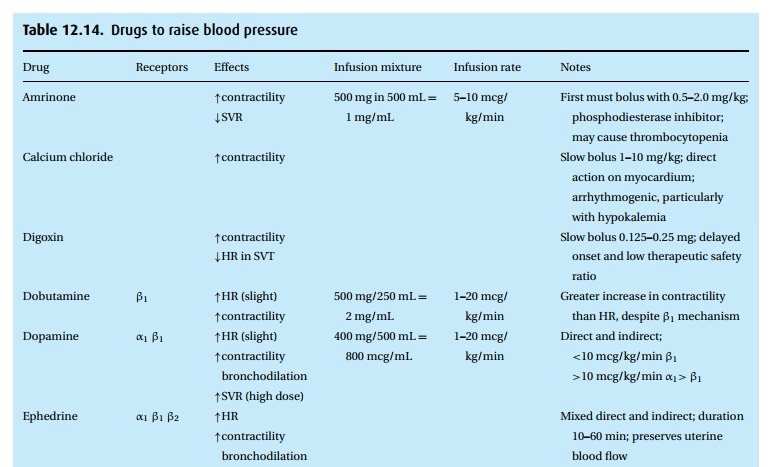
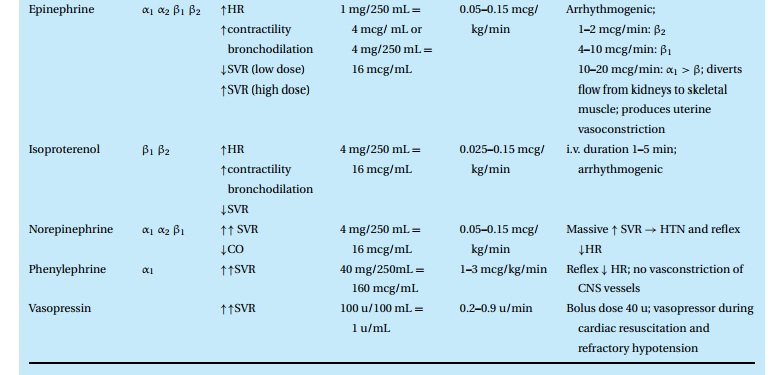
Drugs to raise blood pressure
(Table 12.14)
Hypotension
is initially treated with intravenous fluids, lightening of anesthesia, and
asking the surgeon not to compress major vessels such as the vena cava (if that
was responsible for reducing preload). Sometimes elevating the legs and thereby
increasing venous return can help to improve cardiac output and arterial blood
pressure. In addition, several drugs are available to improve myocardial
con-tractility, increase arterial resistance, and decrease venous capacitance
through adrenergic effects (Table 12.14).
Ephedrine
The old standby still finds common use. We rely on its three-armed effects, alpha and beta stimulation as well as a release of norepinephrine from postganglionic sympathetic nerve terminals. Ten to 20 mg intravenously will increase heart rate and arterial pressure and stimulate the CNS, which we usually do not observe when we give the drug during anesthesia. It has a duration of action of about 20 minutes.
Epinephrine/norepinephrine
Epinephrine
(adrenalin in Britain) and norepinephrine (and noradrenalin) are the two
catecholamines we find circulating in blood. Norepinephrine is liberated from
sympathetic nerve terminals and the adrenal medulla, while epinephrine comes
only from the adrenal gland. Chemically, these two transmitter substances are
identical but for a methyl group on the amine gracing epinephrine but not norepinephrine (NOR=N Ohne (German for “without”) Radical). The drugs dowhat
sympathetic stimulation does. Being physiologic transmitter substances, these
catecholamines have a fleeting effect. Single bolus injections last only for a
matter of a few minutes.
The body
makes extensive use of these catecholamines when fight, fright, or flight call
for cardiovascular, pulmonary, muscular, ocular, and intestinal adjust-ments.
It is amazing how well these substances with overlapping adrenergic effects
orchestrate their actions to an optimal end-result of sympathetic stimulation.
Clinically, we are limited to giving one drug or the other, counting on just
one or the other effect. For example, low doses of epinephrine may reduce blood
pressure a little through a beta2 effect, while larger doses raise
pressure and accelerate heart rate. With norepinephrine, we see primarily
increased pressure without tachycar-dia – as long as the baroreceptors are
active. Typical doses used in the operating room might start with 10 to 20 mcg
of epinephrine as a single i.v. bolus to help the average adult patient through
a spell of hypotension, for example during ana-phylaxis. Usually reserved for
more dire situations, we titrate a norepinephrine infusion to effect, starting
perhaps with 0.1 mcg/kg/min. Epinephrine can also be given by continuous
infusion. During cardiac resuscitation when we assume the body to have become
very much less responsive to circulating catecholamines, doses as high as 1 mg
epinephrine as a bolus have been used.
Dopamine
A
biochemical forerunner to norepinephrine, dopamine also finds clinical use. It
has the – undeserved – aura that in low rates of infusion, e.g., 1–3
mcg/kg/min, it can support blood pressure while maintaining renal perfusion and
promoting diuresis. In larger concentrations, it turns into a vasopressor with
renal vaso-constriction, just as norepinephrine, which it can liberate from
post-ganglionic sympathetic terminals.
Dobutamine (Dobutrex®)
A synthetic catecholamine, dobutamine is a selective β1 agonist with greater effect on contractility than heart rate. It improves cardiac output in patients in cardiac failure. Because of its rapid metabolism, we administer dobutamine as an infusion at 2 to 10 mcg/kg/min, titrated to effect.
Isoproterenol (Isuprel®)
Another
synthetic catecholamine, isoproterenol activates both β1 and β2
recep-tors with great vigor (2–10 times the potency of epinephrine). We use
this agent to (i) increase heart rate, (ii) decrease pulmonary vascular
resistance, andrarely, bronchodilate (i.v. or as an aerosol). Typical of β1
agonism, heart rate, contractility and cardiac output increase while β2
vasodilation reduces SVR. The net effect is a fall in diastolic and mean blood
pressures. Isoproterenol also induces arrhythmias.
Phenylephrine (Neosynephrine®)
An old
standby, phenylephrine sees vasoconstrictive service in nose drops and as an
intravenous, pure α1 agonist. We expect to see both venous and
arterial vasoconstriction with the typical intravenous bolus of 40 to 100 mcg,
which should raise blood pressure for about 5 minutes. Because of its
relatively short duration of effect, we can also infuse it at a rate of about
10 to 100 mcg/min (titrated to effect). Lacking effects at the β receptors, the
drug will not increase heart rate or contractile force. Instead, a baroreceptor
response can lead to lower heart rates.
Related Topics