Chapter: Essential Anesthesia From Science to Practice : Applied physiology and pharmacology : A brief pharmacology related to anesthesia
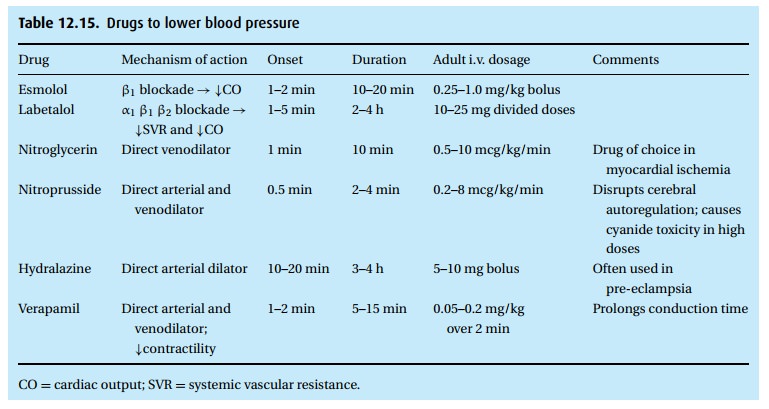
Drugs to lower blood pressure
Drugs to lower blood pressure
(Table 12.15)
While
deepening the anesthetic or adding opioids will correct hypertension from light
anesthesia, many patients require further blood pressure control. We have many
agents at our disposal, with varying mechanisms of action.
Beta blockers
The
older propranolol (Inderal®) was not selective and blocked both β1
and β2 receptors, thus getting some patients into trouble with
bronchoconstriction. Nevertheless, when it became available it represented a
major advance in the treatment of hypertension, myocardial ischemia, and
ventricular arrhythmias.
Frequently
used today are labetalol (Normodyne®; Trandate®) and esmolol (Brevibloc®), two
beta-blockers selective for the β1 receptors with just a weak β2
blocking component. Labetalol has the added advantage of some α1
blocking effect, perhaps 1/7th as strong as its β1 effect, thus
enhancing its antihypertensive action with a little peripheral vasodilatation.
It has a long duration of action, lasting several hours. Typical intravenous
doses start with 10 mg for the average adult. If necessary, these doses can be
repeated in 2- or 3-minute intervals, three or four times.
Esmolol
has two characteristics that make it useful in special circumstances: it exerts
a prominent effect on heart rate and has a rapid onset and relatively short
duration with a half-life of under 10 minutes. The typical bolus dose is
0.25–1.0 mg/kg while infusions of 50 mcg/kg/min may be used for a more
sustained effect.
Beta
blockers are widely used in anesthesia where the common tachycardia sec-ondary
to surgical stimulation or with tracheal intubation can lead to a mismatch of
myocardial oxygen supply (reduced time for coronary perfusion) and demand
(tachycardia, particularly when matched with hypertension). In addition to its
intra-operative use, several studies have demonstrated that prophylactic use of
beta blockers, e.g., metoprolol, throughout the perioperative period reduces
car-diac morbidity and mortality. This is particularly true for patients with
coronary artery disease.
When an
elevated blood pressure cannot, or should not, be lowered by beta blockade or
by deepening anesthesia, and particularly when we wish to have minute-to-minute
control of blood pressure, we need agents with rapid onset of action and short
duration. To meet this need routinely, the body liberates nitric oxide from the
vascular endothelium, which has a fleeting effect of relaxing vas-cular smooth
muscle. Two frequently used drugs, nitroglycerin and nitroprusside, appear to
work by forming nitric oxide, so intimately involved in the tone of blood
vessels. Both drugs take effect within a minute and will dissipate within 5
minutes. A direct vasodilating hypotensive agent, hydralazine (Apresoline®),
finds less use because of its slow onset (up to 10 minutes) and its long
duration (up to 4 hours) of action. However, its long, safe track record makes
it a favorite in the obstetric suite.
Nitroglycerin
Widely
used in cardiology in the treatment of angina, nitroglycerin dilates vascular
smooth muscle, with a preponderance of effect on venous over arterial vessels.
For angina, a typical dose might be a 0.4 mg tablet under the tongue. As a
hypotensive agent to lessen intraoperative bleeding, we infuse nitroglycerin intravenously
at a rate of 0.5 to 1 mcg/kg/min. It is important to permit such low doses time
to show their effect before adjusting the dose upward (potentially up to 10
mcg/kg/min in tolerant patients) in order to avoid hypotension and a stormy up
and down of blood pressure by impatiently adjusting the infusion rate.
Nitroglycerin
has the reputation of relieving coronary spasm and subendo-cardial ischemia,
and thus it finds use when ST-segment depression or flipped T waves signal
myocardial distress. Reduced ventricular pressure and cardiac out-put, without
a marked rise in heart rate, help to re-establish a favorable balance of
myocardial oxygen demand and supply.
Sodium nitroprusside (Nipride®)
In doses
similar to those for nitroglycerin, i.e., starting an infusion of 0.5 to 2
mcg/kg/min and up to 10 mcg/kg/min, if needed, nitroprusside appears to have a
more pronounced effect on arterial vessels and the pulmonary vascular bed than
nitroglycerin. In the brain, sodium nitroprusside dilates vessels and interferes
with autoregulation, which can present problems to patients at risk of
increased intracranial pressure. The biotransformation of nitroprusside can
lead to methemoglobinemia and, in extreme cases, to the liberation of cyanide.
To minimize the chance of this toxicity, we monitor the total dose and keep it
well below 0.5 mg/kg/h.
Clonidine (Catapres®)
Clonidine
occupies an interesting position in the classical scheme of drugs. On the one
hand, it looks a little like a catecholamine, without chemically belonging to
this category; on the other hand, it stimulates alpha adrenergic receptors –
but α2 instead of α1. Thus, it inhibits adrenergic
stimulation and decreases sympa-thetic influence on the heart and peripheral
vascular bed, resulting in bradycardia and hypotension. As such, the drug finds
use in the treatment of hypertension. Anesthesiologists must be aware that the
sudden discontinuation of clonidine medication can trigger rebound
hypertension.
Clonidine
also produces mild sedation and analgesia. It has been used both orally and
mixed with local anesthetics to enhance and prolong analgesia (see Local
anesthetic additives).
Nitric oxide
This interesting gas hides behind a mouthful term, namely the “endothelium-derived relaxing (vasodilatory) factor” or EDRF for short. Its precursors reside in neurons, vascular endothelium, and macrophages. Once synthesized intracellu-larly, the very short-lived nitric oxide (NO) triggers a cascade of steps leading to the relaxation of vascular smooth muscle. As soon as a potential therapeutic role of NO had been appreciated – without a full understanding of its different physiologic roles – industry made it available as a gas that now finds application in treatment of patients with acute respiratory distress syndrome (ARDS). Short-term inhala-tion of tiny concentrations of NO (about 20 ppm) appears to be beneficial in this difficult clinical syndrome.
Related Topics