Chapter: Clinical Dermatology: Connective tissue disorders
Discoid lupus erythematosus
Discoid
lupus erythematosus
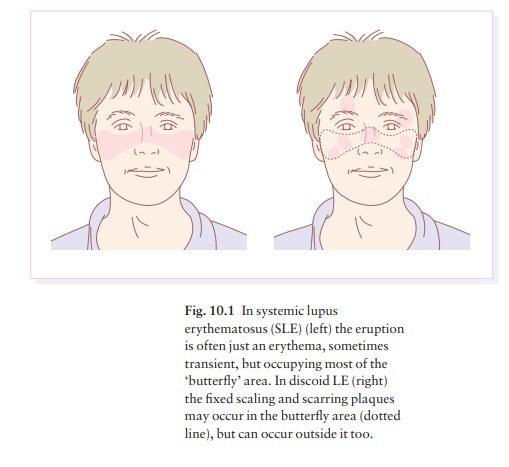
This is the most common form of LE. Patients with discoid LE may have one or two plaques only, or many in several areas. The cause is also unknown but UVR is one factor.
Presentation
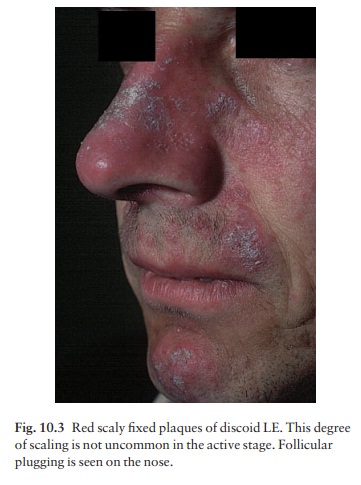
Plaques
show erythema, scaling, follicular plugging (like a nutmeg grater), scarring
and atrophy, telan-giectasia, hypopigmentation and a peripheral zone of
hyperpigmentation. They are well demarcated and lie mostly on sun-exposed skin
of the scalp, face and ears (Figs 10.1 and 10.3). In one variant (chilblain LE)
dusky lesions appear on the fingers and toes.
Course
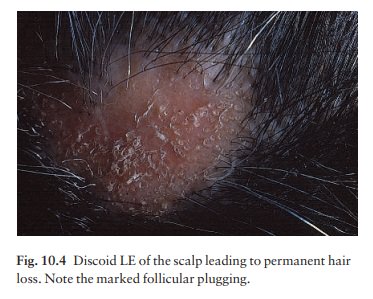
The
disease may spread relentlessly, but in about half of the cases the disease
goes into remission over the course of several years. Scarring is common and
hair may be lost permanently if there is scarring in the scalp (Fig. 10.4).
Whiteness remains after the inflammation has cleared, and hypopigmentation is
common in dark-skinned people. Discoid LE rarely progresses to SLE.
Differential diagnosis
Psoriasis
is hard to tell from discoid LE when its plaques first arise but has larger
thicker scales, and later it is usually symmetrical and affects sites different
from
Discoid LE is more common on the face and ears, and in
sun-exposed areas, whereas psoriasis favours the elbows, knees, scalp and
sacrum. Discoid LE is far more prone than psoriasis to scar and cause hair
loss. Jessner’s lymphocytic infiltration is best viewed as a dermal form of
discoid LE.
Investigations
Most patients with discoid LE remain well. However, screening for SLE and internal disease is still worth-while. A skin biopsy is most helpful if taken from an untreated plaque where appendages are still present.
Treatment
Discoid
LE needs potent or very potent topical corti-costeroids. In this condition, it
is justifiable to use them on the face, as the risk of scar-ring is worse than
that of atrophy. Topical steroids should be applied twice daily until the
lesions disappear or side-effects, such as atrophy, develop; weaker
pre-parations can then be used for maintenance. If discoid LE does not respond
to this, intralesional injections of triamcinolone (2.5 or 10 mg/mL) may help.
Stubborn and widespread lesions often do well with oral anti-malarials such as
hydroxychloroquine, but rarely these cause irreversible eye dam-age. The eyes
should therefore be tested before and at intervals during treatment. Sun
avoidance and screens are also important. Oral retinoids and thalidomide have
proved helpful in stubborn cases but a specialist, with experience of their
use, should prescribe these controlled treatments and supervise management.
Related Topics