Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Disorders
Common Problems of the Upper Extremity
Common
Problems of the Upper Extremity
The structures in the upper extremity are frequently the
sites of painful syndromes. The structures most frequently affected are the
shoulder, wrist, and hand.
BURSITIS AND TENDINITIS
Bursitis and tendinitis are inflammatory conditions
that com-monly occur in the shoulder. Bursae are fluid-filled sacs that
pre-vent friction between joint structures during joint activity. When
inflamed, they are painful. Similarly, muscle tendon sheaths be-come inflamed
with repetitive stretching. The inflammation causes proliferation of synovial
membrane and pannus formation, which restricts joint movement. Conservative
treatment includes rest of the extremity, intermittent ice and heat to the
joint, and nonsteroidal anti-inflammatory drugs (NSAIDs) to control the
inflammation and pain. Arthroscopic synovectomy may be con-sidered if shoulder
pain and weakness persist.
LOOSE BODIES
Loose bodies may occur
in a joint as a result of articular cartilage wear and bone erosion. These
fragments interfere with joint movement, locking the joint, and cause painful
movement. Loose bodies are removed by arthroscopic surgery.
IMPINGEMENT SYNDROME
Overuse (microtrauma) may produce an impingement syndrome
in the shoulder. The supraspinatus and biceps tendons become irritated and
edematous and press against the acromion process, limiting shoulder motion. The
patient experiences pain, shoulder tenderness, limited movement, muscle spasm,
and atrophy. The process may progress to a rotator cuff tear. Conservative
treat-ment includes rest, NSAIDs, joint injections, and physical ther-apy
(Chart 68-4). Arthroscopic débridement is used for persistent pain. Gentle
joint motion is begun after surgery.
CARPAL TUNNEL SYNDROME
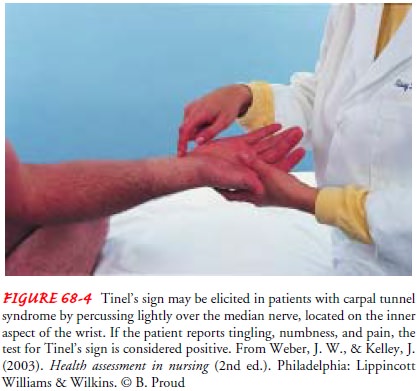
Carpal tunnel syndrome
is an entrapment neuropathy that occurs when the median nerve at the wrist is
compressed by a thickened flexor tendon sheath, skeletal encroachment, edema,
or a soft tis-sue mass. The syndrome is commonly caused by repetitive hand
activities but may be associated with arthritis, hypothyroidism, or pregnancy.
The patient experiences pain, numbness, paresthesia, and possibly weakness
along the median nerve (thumb and first two fingers). Tinel’s sign may be used
to help identify carpal tun-nel syndrome (Fig. 68-4). Night pain is common.
Treatment is based on cause. Rest splints to prevent hyperextension and
pro-longed flexion of the wrist, avoidance of repetitive flexion of the wrist
(eg, use of ergonomic changes at work to reduce wrist strain), NSAIDs, and
carpal canal cortisone injections may relieve the symptoms. Specific yoga
postures, relaxation, and acupuncture may provide nontraditional alternatives
to relieve carpal tunnel symptoms. Traditional or endoscopic laser surgical
release of the transverse carpal ligament may be necessary. The patient wears a
hand splint after surgery and limits hand use during healing. The patient may
need assistance with personal care and ADLs. Full re-covery of motor and
sensory function after nerve release surgery may take several weeks or months.
GANGLION
A ganglion, a collection of gelatinous material near the tendon sheaths and joints, appears as a round, firm, cystic swelling, usu-ally on the dorsum of the wrist. It most frequently occurs in women younger than 50 years of age. The ganglion is locally ten-der and may cause an aching pain. When a tendon sheath is in volved, weakness of the finger occurs. Treatment may include as-piration, corticosteroid injection, or surgical excision. After treat-ment, a compression dressing and immobilization splint are used.
DUPUYTREN’S CONTRACTURE
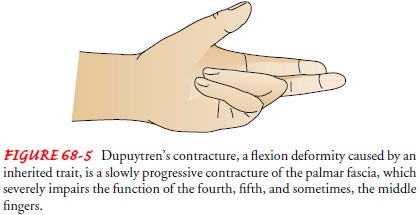
Dupuytren’s deformity is
a slowly progressive contra1cture of
the palmar fascia, which causes flexion of the fourth and fifth fingers, and
frequently the middle finger. This renders the fingers more or less useless
(Fig. 68-5). It is caused by an inherited autosomal dominant trait and occurs
most frequently in men who are older than 50 years of age and who are of
Scandinavian or Celtic ori-gin. It is also associated with arthritis, diabetes,
gout, and alco-holism. It starts as a nodule of the palmar fascia. The nodule
may not change, or it may progress so that the fibrous thickening ex-tends to
involve the skin in the distal palm and produces a con-tracture of the fingers.
The patient may experience dull aching discomfort, morning numbness, cramping,
and stiffness in the affected fingers. This condition starts in one hand, but
eventu-ally both hands are affected symmetrically. Initially, finger-stretching
exercises may prevent contractures. With contracture development, palmar and
digital fasciectomies are performed to improve function. Finger exercises are
begun on postoperative day 1 or 2.
Related Topics