Chapter: Medical Surgical Nursing: Management of Patients With Upper or Lower Urinary Tract Dysfunction
Urinary Retention - Dysfunctional Voiding Patterns
URINARY
RETENTION
Urinary
retention is the inability to empty the bladder completely during attempts to
void. Chronic urine retention often leads to overflow incontinence (from the
pressure of the retained urine in the bladder). Residual urine is urine that
remains in the bladder after voiding. In a healthy adult younger than age 60,
complete bladder emptying should occur with each voiding. In adults older than
age 60, 50 to 100 mL of residual urine may remain after each void because of
the decreased contractility of the detrusor muscle.
Urinary
retention can occur postoperatively in any patient, particularly if the surgery
affected the perineal or anal regions and resulted in reflex spasm of the
sphincters. General anesthesia re-duces bladder muscle innervation and
suppresses the urge to void, impeding bladder emptying (Gray, 2000a, 2000b).
Pathophysiology
Urinary
retention may result from diabetes, prostatic enlarge-ment, urethral pathology
(infection, tumor, calculus), trauma (pelvic injuries), pregnancy, or
neurologic disorders such as cere-brovascular accident, spinal cord injury,
multiple sclerosis, or Parkinson’s disease.
Some medications cause urinary retention, either by inhibiting bladder contractility or by increasing bladder outlet resistance. Medications that cause retention by inhibiting bladder contractil-ity include anticholinergic agents (atropine sulfate, dicyclomine hydrochloride [Antispas, Bentyl]), antispasmodic agents (oxybu-tynin chloride [Ditropan], belladonna, and opioid suppositories), and tricyclic antidepressant medications (imipramine [Tofranil], doxepin [Sinequan]). Medications that cause urine retention by increasing bladder outlet resistance include alpha-adrenergic agents (ephedrine sulfate, pseudoephedrine), beta-adrenergic blockers (propranolol), and estrogens.
PROMOTING URINARY ELIMINATION
When
the patient cannot void, catheterization is used to prevent overdistention of
the bladder (see later discussion of neurogenic bladder and catheterization).
In the case of prostatic obstruction, attempts at catheterization (by the
urologist) may not be successful, requiring insertion of a suprapubic catheter. After urinary drainage is restored, bladder
retraining is initiated for the patient who can-not void spontaneously.
PROMOTING HOME AND COMMUNITY-BASED CARE
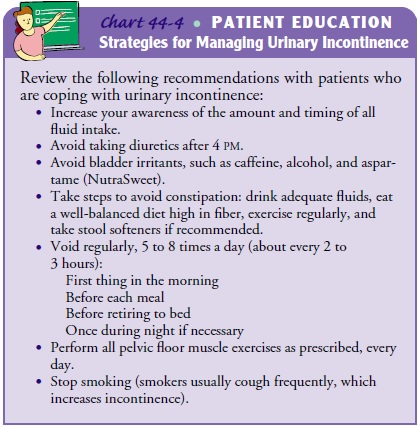
Modifying
the home environment is a simple and effective way to treat urinary
incontinence. In adapting the home environment to provide easy, safe access to
the bathroom, the patient may need to remove barriers, such as throw rugs or
other objects, from the route. Other modifications that the nurse may recommend
in-clude installing support bars in the bathroom and placing a bed-pan or
urinal within easy reach. Leaving a light on in the bedroom and bathroom and
wearing clothing that is easy to remove when using the toilet are other
recommendations (see Chart 44-4).
Gerontologic Considerations
If
nurses and other health care providers accept incontinence as an inevitable
part of illness or aging or consider it irreversible and untreatable at any
age, it cannot be treated successfully. Collabo-rative, interdisciplinary
efforts are essential in assessing and effec-tively treating urinary
incontinence.
Related Topics