Chapter: Medical Surgical Nursing: Management of Patients With Upper or Lower Urinary Tract Dysfunction
Kidney Surgery
Kidney Surgery
A
patient may undergo surgery to remove obstructions that affect the kidney
(tumors or calculi), to insert a tube for draining the kidney (nephrostomy, ureterostomy), or to
remove the kidney involved in unilateral kidney disease, renal carcinoma, or
kidney transplantation.
PREOPERATIVE CONSIDERATIONS
Surgery
is performed only after a thorough evaluation of renal function. Patient
preparation to ensure that optimal renal func-tion is maintained is mandatory.
Fluids are encouraged to promote increased excretion of waste products before
surgery, unless con-traindicated because of preexisting renal or cardiac
dysfunction. If kidney infection is present preoperatively, wide-spectrum
anti-microbial agents may be prescribed to prevent bacteremia. Anti-biotic
agents must be given with extreme care because many are toxic to the kidneys. Coagulation
studies (prothrombin time, par-tial thromboplastin time, platelet count) may be
indicated if the patient has a history of bruising and bleeding.
Because
many patients facing kidney surgery are apprehensive, the nurse encourages the
patient to recognize and express any feelings of anxiety. Confidence is
reinforced by establishing a re-lationship of trust and by providing expert
care. Patients faced with the prospect of losing a kidney may think that they
will be dependent on dialysis for the rest of their life. It is important to
teach the patient and family that normal function may be main-tained by a
single healthy kidney.
PERIOPERATIVE CONCERNS
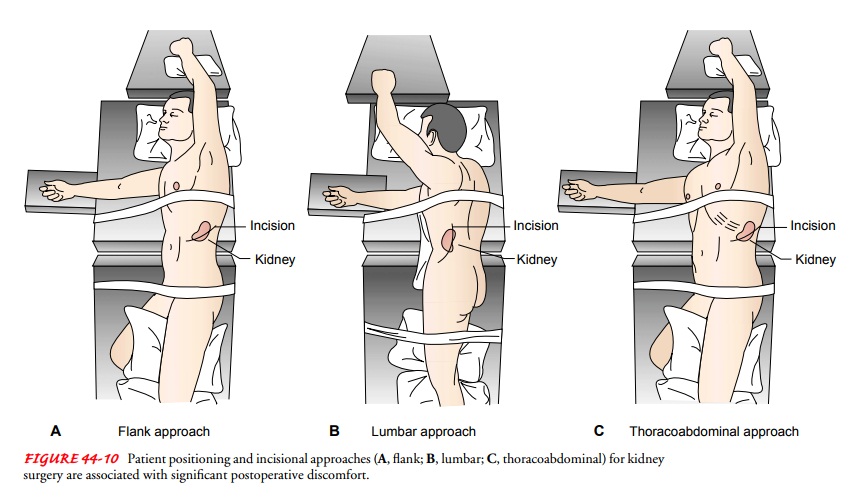
Renal
surgery requires various patient positions to expose the sur-gical site
adequately. Three surgical approaches are common: flank, lumbar, and
thoracoabdominal (Fig. 44-10). During surgery, plans are carried out for
managing altered urinary drainage and drainage systems. Plans may include
inserting a nephrostomy or other drainage tube or using ureteral stents.

POSTOPERATIVE MANAGEMENT
Because
the kidney is a highly vascular organ, hemorrhage and shock are the chief
complications of renal surgery. Fluid and blood component replacement is
frequently necessary in the im-mediate postoperative period to treat
intraoperative blood loss.
Abdominal
distention and paralytic ileus are fairly common after renal and ureter surgery
and are thought to be due to a re-flex paralysis of intestinal peristalsis and
manipulation of the colon or duodenum during surgery. Abdominal distention is
re-lieved by decompression through a nasogastric tube. Oral fluids are
permitted when the passage of flatus is noted.
If
infection occurs, antibiotic agents are prescribed after a cul-ture reveals the
causative organism. The toxic effects that anti-biotic agents have on the
kidneys (nephrotoxicity) must be kept in mind when assessing the patient.
Low-dose heparin therapy may be initiated postoperatively to prevent
thromboembolism in patients who had any type of urologic surgery.
Drainage Tubes
Almost
all patients undergoing kidney and urologic surgery, as well as patients with
other kidney and urologic disturbances, have drains, tubes, or catheters in
place. All catheters and tubes must be kept patent (eg, draining) to prevent obstruction
by blood clots, which can cause infection, kidney damage, or severe pain
(similar to renal colic) when they pass along the ureter.
Nephrostomy Drainage
A
nephrostomy tube is inserted directly into the kidney for tem-porary or
permanent urinary diversion. It can be inserted either percutaneously or
through a surgical incision. A single tube or a self-retaining U loop or
circular nephrostomy tube may be used and is attached to a closed drainage
system or to a urostomy appliance. Nephrostomy drainage may be required to
provide drainage from the kidney after surgery or to bypass an obstruc-tion in
the ureter or lower urinary tract. Permanent nephrostomy tubes are usually
changed every 3 months.
Percutaneous
nephrostomy is the insertion of a tube through the skin into the renal pelvis.
This procedure is performed to pro-vide external drainage of urine from an
obstructed ureter, to create a route for inserting a ureteral stent (see
following discussion), to dilate strictures, to close fistulas, to administer
medications, to allow insertion of a brush biopsy instrument and nephroscope,
or to perform selected surgical procedures.
The skin site is prepared and anesthetized, and the patient is asked to inhale and hold his or her breath while a spinal needle is advanced into the renal pelvis. Urine is aspirated for culture, and a contrast agent may be injected into the pyelocalyceal system. An angiographic catheter guide wire is introduced through the nee-dle to the kidney. The needle is withdrawn and the tract dilated by the passage of tubes or guide wires. The nephrostomy tube is introduced and positioned within the kidney or ureter, fixed by skin sutures, and connected to a closed drainage system.
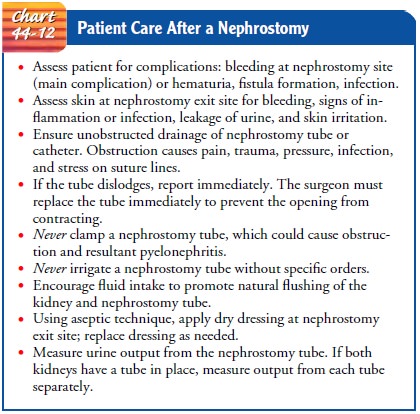
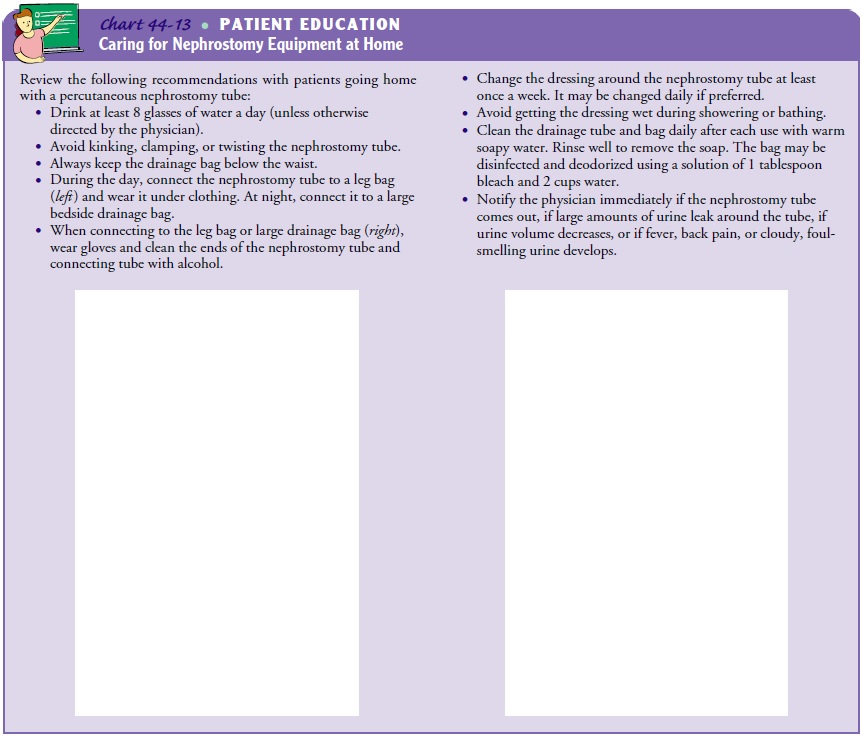
Before
a percutaneous nephrostomy tube is inserted, several precautions should be
taken. The patient should receive a broad-spectrum antibiotic to prevent
infection. Bleeding disorders and uncontrolled hypertension should be
corrected. Also, anticoagu-lant agents and aspirin should be discontinued and
bleeding study results (prothrombin time, partial thromboplastin time, platelet
count) should be normal to decrease the chance of devel-oping a perirenal
hematoma or renal hemorrhage. Chart 44-12 describes postsurgical nursing care
of the patient with a nephros-tomy tube (also see Chart 44-13).
Ureteral Stents
A
ureteral stent is a self-retaining tubular device that helps main-tain the
position and patency of the ureter. Stents are used to maintain urine flow in
patients with ureteral obstruction (from edema, stricture, fibrosis, calculi,
or tumors), to divert urine, to promote healing, and to maintain the caliber
and patency of the ureter after surgery (Fig. 44-11). Stents are usually
removed 4 to 6 weeks after surgery in an outpatient setting without the need
for general anesthesia or risk of ureteral injury.
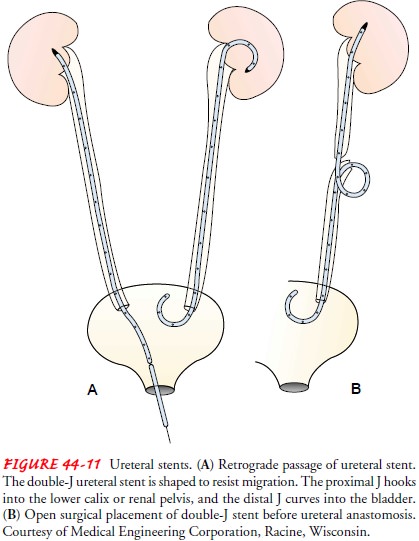
The
stent, usually made of soft, flexible silicone, may be inserted through a
cystoscope or nephrostomy tube or by open surgery. Complications include
infection, inflammation secondary to a for-eign body in the genitourinary
tract, tube encrustation, bleeding or clot obstruction within the stent, and
migration or displacement of the stent (Lehmann & Dietz, 2002).
Several
stents are designed to avoid some of these problems. The double-J ureteral
stent has a J-shaped curve molded into each end that prevents upward or
downward migration. This stent can be used in place of a nephrostomy for short-
or long-term urinary drainage. The double-pigtail ureteral stent has a pigtail
coil at each end; this permits placement of the upper coil (pigtail) in the
renal pelvis, with the lower coil at the ureteral orifice. The coils prevent
the stent from moving and allow free body movement.
Nursing interventions related to the care of a patient with a ureteral stent include monitoring the patient for bleeding, assess-ing and measuring urine output, assessing the patient for signs of urinary
tract infection or retroperitoneal infection from leakage of urine, and
monitoring the patient for stent displacement, which is evidenced by colicky
pain and a decrease in urine out-put. An indwelling stent may produce a local
ureteral reaction, including mucosal edema, which can cause temporary
obstruc-tion of the ureter and intense pain.
Related Topics