Chapter: Medical Surgical Nursing: Management of Patients With Upper or Lower Urinary Tract Dysfunction
Continuous Renal Replacement Therapies - Dialysis
CONTINUOUS
RENAL REPLACEMENT THERAPIES
Several
types of continuous renal replacement
therapy (CRRT) are available and are widely used in critical care units.
CRRT may be indicated for patients who have acute or chronic renal failure and
who are too clinically unstable for traditional hemodialysis, for patients with
fluid overload secondary to oliguric (low urine output) renal failure, and for
patients whose kidneys cannot han-dle their acutely high metabolic or
nutritional needs. CRRT does not produce rapid fluid shifts, does not require
dialysis machines or dialysis personnel to carry out the procedures, and can be
ini-tiated quickly in hospitals without dialysis facilities.
CRRT
methods are similar to hemodialysis methods in that they require access to the
circulation and blood to pass through an artificial filter. A hemofilter (an
extremely porous blood filter containing a semipermeable membrane) is used in
all CRRT methods, which are described below (Astle, 2001).
Continuous Arteriovenous Hemofiltration
Continuous arteriovenous hemofiltration (CAVH) was firstused in 1977 to
treat fluid overload. Blood is circulated through a small-volume,
low-resistance filter, using the patient’s arterial pressure rather than that
of the blood pump as is used in he-modialysis. Blood flows from an artery
(usually by an arterial catheter in the femoral artery) to a hemofilter. A
pressure gradi-ent is necessary for optimal filtration; cannulation of the
femoral artery and vein provides the necessary gradient (difference) in
ar-terial and venous pressures. The filtered blood then returns to the
patient’s circulation through a venous catheter. Intravenous flu-ids may be
administered to replace fluid removed by the proce-dure. With CAVH, there is no
concentration gradient, so only fluid is filtered. Electrolytes are eliminated
only as they are pulled along and removed with the fluid. Ultrafiltrate is
collected in a drainage bag, measured, and discarded. CAVH is usually set up
and initiated by trained dialysis staff and then maintained and monitored by
critical care personnel.
Continuous Arteriovenous Hemodialysis
Continuous arteriovenous hemodialysis (CAVHD) has manyof the
characteristics of CAVH but offers the advantage of a concentration gradient
for faster clearance of urea. This is ac-complished by the circulation of
dialysate on one side of a semi-permeable membrane. The blood flow through the
system depends on the patient’s arterial pressure, as in CAVH; a blood pump is
not used as it is in standard hemodialysis. CAVHD is usually set up and
initiated by trained dialysis staff and then maintained and monitored by
critical care personnel.
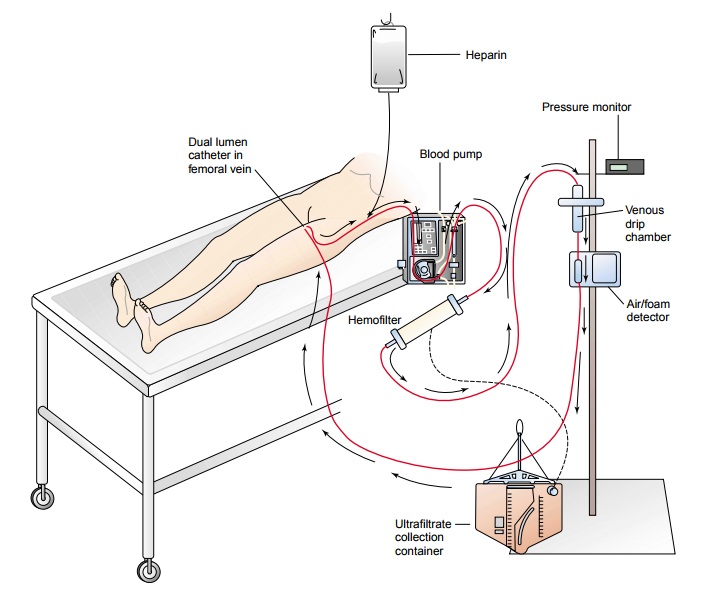
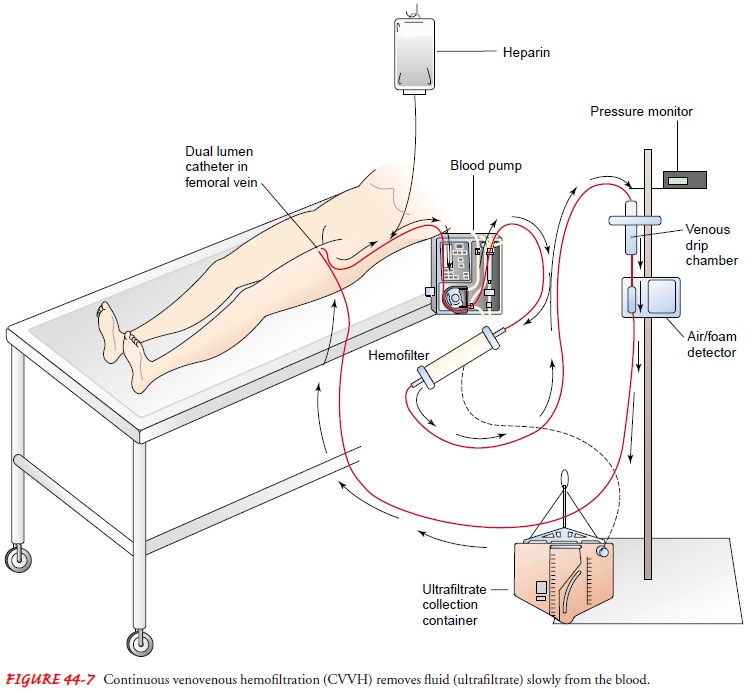
Continuous Venovenous Hemofiltration
Continuous venovenous hemofiltration (CVVH) is increas-ingly being
used in managing acute renal failure. Blood from a double-lumen venous catheter
is pumped (using a small blood pump) through a hemofilter and then returned to
the patient through the same catheter (Fig. 44-7). CVVH provides continu-ous
slow fluid removal (ultrafiltration); therefore, hemodynamic effects are mild
and better tolerated by patients with unstable conditions. CVVH has several
other benefits over CAVH in that no arterial access is required and critical
care nurses can set up, initiate, maintain, and terminate the system.
Continuous Venovenous Hemodialysis
Continuous venovenous hemodialysis (CVVHD) is similar toCVVH. Blood
is pumped from a double-lumen venous catheter through a hemofilter and returned
to the patient through the same catheter. In addition to the benefits of
ultrafiltration, CVVHD uses a concentration gradient to facilitate the removal
of uremic toxins. Therefore, no arterial access is required, hemodynamic
effects are usually mild, and critical care nurses can set up, ini-tiate,
maintain, and terminate the system.
Related Topics