Chapter: Medical Surgical Nursing: Management of Patients With Upper or Lower Urinary Tract Dysfunction
Urinary Incontinence - Dysfunctional Voiding Patterns
URINARY
INCONTINENCE
More
than 17 million adults in the United States are estimated to have urinary
incontinence, with most of them experiencing over-active bladder syndrome,
making this disorder more prevalent than diabetes or ulcer disease. Despite
widespread media coverage, urinary incontinence remains underdiagnosed and
underreported. Patients may be too embarrassed to seek help, causing them to
ignore or conceal symptoms. Many patients resort to using ab-sorbent pads or
other devices without having their condition prop-erly diagnosed and treated.
Health care providers must be alert to subtle cues of urinary incontinence and
stay informed about cur-rent management strategies.
The
costs of care for patients with urinary incontinence are not limited to the
dollars spent for absorbent products, medications, and surgical or nonsurgical
treatment modalities. The psycho-social costs of urinary incontinence are also
significant: embar-rassment, loss of self-esteem, and social isolation are
common outcomes. Urinary incontinence in elderly patients often decreases their
ability to maintain an independent lifestyle. This increases dependence on
caregivers and often leads to institutionalization.
Urinary
incontinence affects people of all ages but is particu-larly common among the
elderly. It has been reported that more than half of all nursing home residents
have urinary incontinence. Although urinary incontinence is not a normal
consequence of aging, age-related changes in the urinary tract predispose the
older person to incontinence.
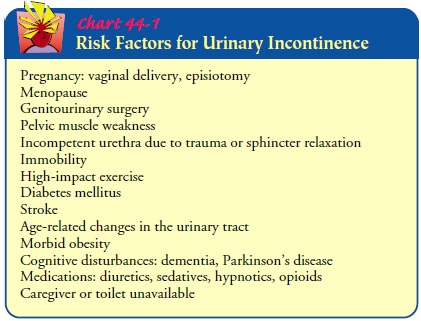
Although
urinary incontinence is commonly regarded as a condition that occurs in older
multiparous women, it is also com-mon in young nulliparous women, especially
during vigorous high-impact activity. Age, gender, and number of vaginal deliv-eries
are established risk factors (Chart 44-1); they explain, in part, the increased
incidence in women. Urinary incontinence is a symptom with many possible
causes.
Clinical Manifestations:Types of Incontinence
Stress incontinence is the involuntary loss of urine through
anintact urethra as a result of a sudden increase in intra-abdominal pressure
(sneezing, coughing, or changing position). It predomi-nately affects women who
have had vaginal deliveries and is thought to be the result of decreasing
ligament and pelvic floor support of the urethra and decreasing or absent
estrogen levels within the urethral walls and bladder base. In men, stress
incon-tinence is often experienced after a radical prostatectomy for prostate
cancer because of the loss of urethral compression that the prostate had
supplied before the surgery, and possibly blad-der wall irritability (Reilly,
2001; Sueppel et al., 2001) (see Nursing Research Profile 44-1).
Urge incontinence is the involuntary loss of urine
associatedwith a strong urge to void that cannot be suppressed. The patient is
aware of the need to void but is unable to reach a toilet in time. An
uninhibited detrusor contraction is the precipitating factor. This can occur in
a patient with neurologic dysfunction that im-pairs inhibition of bladder
contraction or in a patient without overt neurologic dysfunction (Chancellor,
1999).
Reflex incontinence is the involuntary loss of urine due
tohyperreflexia in the absence of normal sensations usually associated with
voiding. This commonly occurs in patients with spinal cord injury because they
have neither neurologically mediated motor control of the detrusor nor sensory
awareness of the need to void.
Overflow incontinence is the involuntary loss of urine asso-ciated
with overdistention of the bladder. Such overdistention results from the
bladder’s inability to empty normally, despite fre-quent urine loss. Both
neurologic abnormalities (eg, spinal cord lesions) and factors that obstruct
the outflow of urine (eg, tumors, strictures, and prostatic hyperplasia) can
cause overflow inconti-nence (Reilly, 2001).
Functional
incontinence refers to those instances in which lower urinary tract function is
intact but other factors, such as se-vere cognitive impairment (eg, Alzheimer’s
dementia), make it difficult for the patient to identify the need to void or
physical impairments make it difficult or impossible for the patient to reach
the toilet in time for voiding.
Iatrogenic
incontinence refers to the involuntary loss of urine due to extrinsic medical
factors, predominantly medications. One such example is the use of
alpha-adrenergic agents to lower blood pressure. In some individuals with an
intact urinary system, these agents adversely affect the alpha receptors
responsible for bladder neck closing pressure; the bladder neck relaxes to the
point of in-continence with a minimal increase in intra-abdominal pressure,
thus mimicking stress incontinence. As soon as the medication is discontinued,
the apparent incontinence resolves (Reilly, 2001).
Some
patients have several types of urinary incontinence. This mixed incontinence is
usually a combination of stress and urge incontinence.
Only
with appropriate recognition of the problem, assess-ment, and referral for diagnostic
evaluation and treatment can the outcome of incontinence be determined. All
people with incon-tinence should be considered for evaluation and treatment.
Assessment and Diagnostic Findings
Once
incontinence is recognized, a thorough history is necessary. This includes a
detailed description of the problem and a history of medication use. The
patient’s voiding history, a diary of fluid intake and output, and bedside
tests (ie, residual urine, stress
maneuvers) may be used to help determine the type of urinary incontinence
involved. Extensive urodynamic tests may be per-formed;. Urinalysis and urine
culture are per-formed to identify hematuria (from infection, cancer, or a
kidney stone), glycosuria (causes polyuria), pyuria, and bacteriuria (bacteria
in the urine), all of which may identify transient causes of urinary
incontinence.
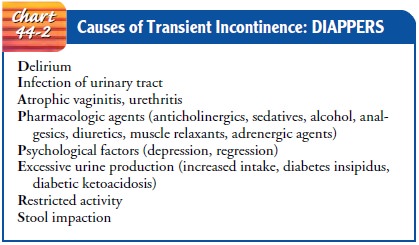
Management
depends on the type of urinary incontinence and its causes. Urinary
incontinence may be transient or re-versible (Chart 44-2), provided that the
underlying cause is suc-cessfully treated and the voiding pattern reverts to
normal. Management of urinary incontinence not considered transient or
reversible falls into three categories: pharmacologic, surgical, and
behavioral.
Gerontologic Considerations
Many
older individuals experience transient episodes of inconti-nence that tend to
be abrupt in onset. When this occurs, the nurse should question the patient, as
well as the family if possi-ble, about the onset of symptoms and any signs or
symptoms of a change in other organ systems.
Acute
urinary tract infection, infection elsewhere in the body, constipation,
decreased fluid intake, a change in a chronic disease pattern, such as elevated
blood glucose levels in patients with di-abetes or decreased estrogen levels in
menopausal women, can provoke the onset of urinary incontinence. If the cause
is identi-fied and modified or eliminated early at the onset of inconti-nence,
the incontinence itself may be eliminated. Although the older bladder is more
vulnerable to unstable detrusor activity, age alone is not a risk factor for
urinary incontinence (Suchinski et al., 1999).
Medical Management
Treatment
of urinary incontinence depends on the underlying cause. Before appropriate
treatment can be initiated, however, the problem and the cause must be
identified.
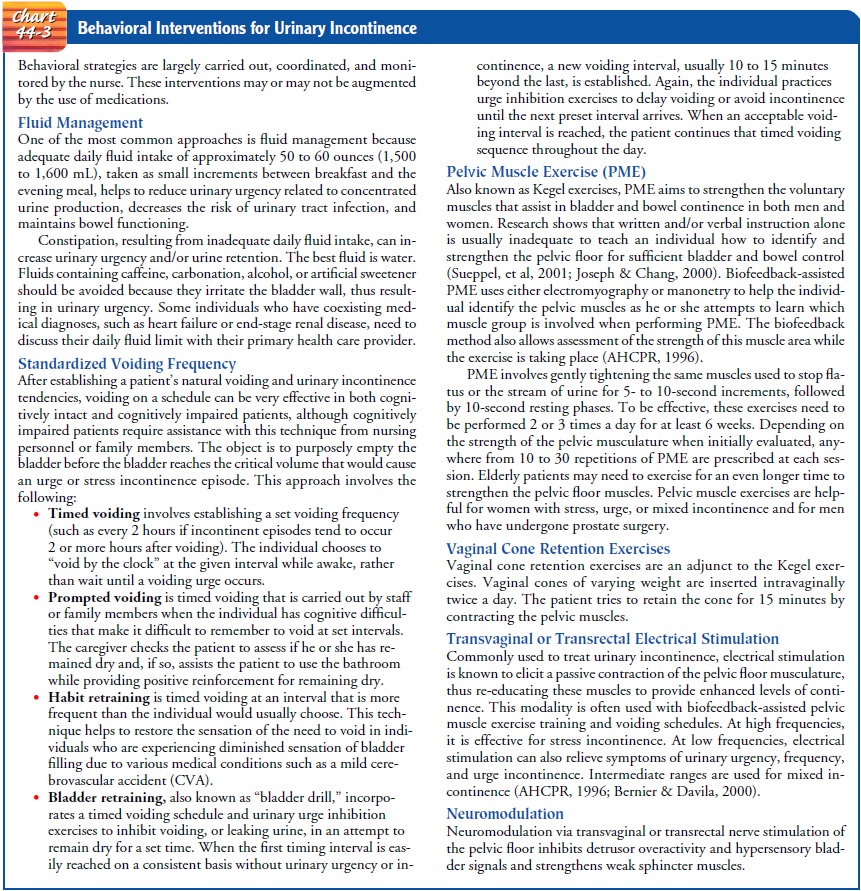
BEHAVIORAL THERAPY
Behavioral
therapies are always the first choice to decrease or eliminate urinary
incontinence. In using these techniques, clini-cians help patients avoid
potential adverse effects of pharmaco-logic or surgical interventions (AHCPR,
1996; Roberts, 2001) (Chart 44-3).
PHARMACOLOGIC THERAPY
Pharmacologic therapy works best when used as an adjunct to behavioral interventions. Anticholinergic agents (oxybutynin [Ditropan],
dicyclomine [Antispas]) inhibit bladder contraction and are considered
first-line medications for urge incontinence. Several tricyclic antidepressant
medications (imipramine, dox-epin, desipramine, and nortriptyline) also
decrease bladder contractions as well as increase bladder neck resistance.
Stress in-continence may be treated using pseudoephedrine (eg, Sudafed).
Estrogen (taken orally, transdermally, or topically) has been shown to be
beneficial for all types of urinary incontinence. Es-trogen decreases
obstruction to urine flow by restoring the mu-cosal, vascular, and muscular
integrity of the urethra.
Gerontologic Considerations
Elderly individuals may experience cognitive decline when taking short-acting anticholinergic medications. The long-acting forms of anticholinergic medications such as oxybutynin (Ditropan XL) and tolterodine (Detrol LA) have a significantly lower inci-dence of adverse effects in all populations, including the elderly (Roberts, 2001).
SURGICAL MANAGEMENT
Surgical
correction may be indicated in patients who have not achieved continence using
behavioral and pharmacologic ther-apy. Surgical options vary according to the
underlying anatomy and the physiologic problem. Most procedures involve lifting
and stabilizing the bladder or urethra to restore the normal urethro-vesical
angle or to lengthen the urethra.
Women
with stress incontinence may have an anterior vagi-nal repair, retropubic
suspension, or needle suspension to reposition the urethra. Procedures to
compress the urethra and increase resistance to urine flow include sling
procedures and placement of periurethral bulking agents such as artificial
collagen.
Periurethral
bulking is a semipermanent procedure in which small amounts of artificial
collagen are placed within the walls of the urethra to enhance the closing
pressure of the urethra. This procedure takes only 10 to 20 minutes and may be
performed under local anesthesia or moderate sedation. A cystoscope is in-serted
into the urethra. An instrument is inserted through the cys-toscope to deliver
a small amount of collagen into the urethral wall at locations selected by the
urologist. The patient is usually discharged home after voiding. There are no
restrictions follow-ing the procedure, although occasionally more than one
collagen bulking session may be necessary if the initial procedure did not halt
the stress urinary incontinence. Collagen placement any-where in the body is
considered semipermanent because its dura-bility averages between 12 and 24
months, until the body absorbs the material. Periurethral bulking with collagen
offers an alterna-tive to surgery, as in a frail, elderly individual. It is
also an option for individuals who are seeking help with stress urinary
inconti-nence who prefer to avoid surgery and who do not have access to
biofeedback and electrical stimulation.
A
modified artificial sphincter that uses a silicone-rubber balloon as a
self-regulating pressure mechanism can be used to close the urethra. Electronic
stimulation of the pelvic floor by means of a miniature pulse generator with
electrodes mounted on an intra-anal plug is another method of controlling
stress in-continence.
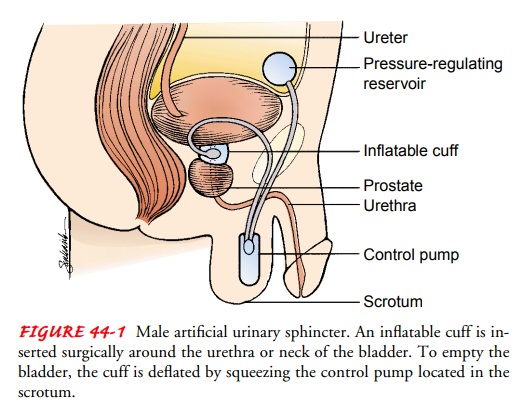
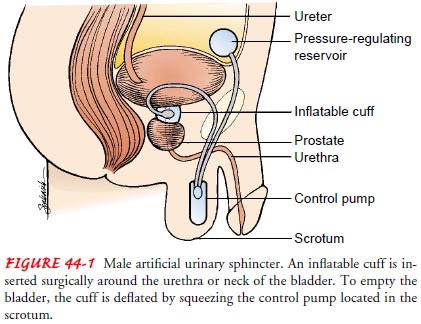
Men
with overflow and stress incontinence may undergo a transurethral resection to
relieve symptoms of prostatic enlarge-ment. An artificial sphincter can be used
after prostatic surgery for sphincter incompetence (Fig. 44-1). After surgery,
peri-urethral bulking agents can be injected into the periurethral area to
increase compression of the urethra.
Nursing Management
Nursing
management is based on the premise that incontinence is not inevitable with
illness or aging and that it is often reversible and treatable. The nursing
interventions are determined in part by the type of treatment that is
undertaken. For behavioral ther-apy to be effective, the nurse must provide
support and encour-agement, because it is easy for the patient to become
discouraged if therapy does not quickly improve the level of continence.
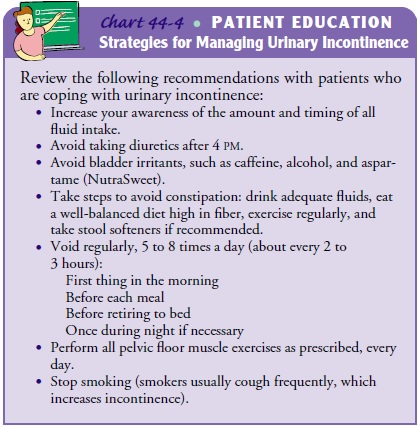
Pa-tient teaching regarding the bladder program is important and should be
provided verbally and in writing (Chart 44-4). The pa-tient is assisted to
develop and use a log or diary to record timing of Kegel exercises, changes in
bladder function with treatment, and episodes of incontinence.
If pharmacologic treatment is used, its purpose is explained to the patient and family. If surgical correction is undertaken, the procedure and its desired outcomes are described to the patient and family. Follow-up contact with the patient enables the nurse to answer the patient’s questions and to provide reinforcement and encouragement. Patients who have mixed incontinence (both stress and urge incontinence) need to understand that anticholinergic and antispasmodic agents can help decrease urinary urgency and frequency and urge incontinence, but they do not decrease the urinary incontinence related to stress incontinence.
Related Topics