Chapter: Basic & Clinical Pharmacology : Diuretic Agents
Thiazides
THIAZIDES
The
thiazide diuretics were discovered in 1957, as a result of efforts to
synthesize more potent carbonic anhydrase inhibitors. It subsequently became
clear that the thiazides inhibit NaCl, rather than NaHCO3−
transport and that their action was predominantly in the DCT, rather than the
PCT. Some members of this group retain significant carbonic anhydrase
inhibitory activity (eg, chlor-thalidone). The prototypical thiazide is hydrochlorothiazide(HCTZ).
Chemistry & Pharmacokinetics
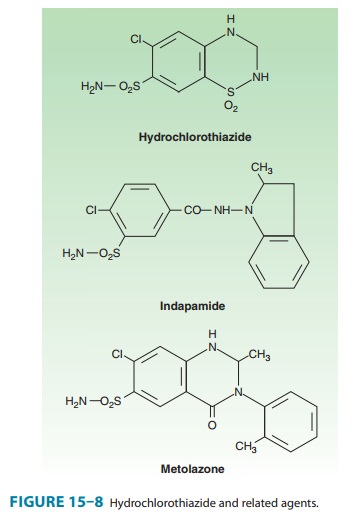
Like
carbonic anhydrase inhibitors and three loop diuretics, all of the thiazides
have an unsubstituted sulfonamide group (Figure 15–8).
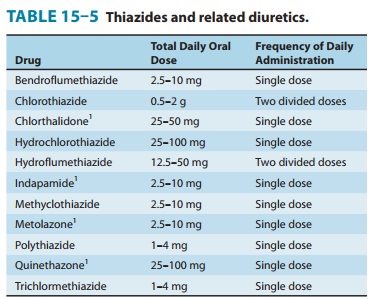
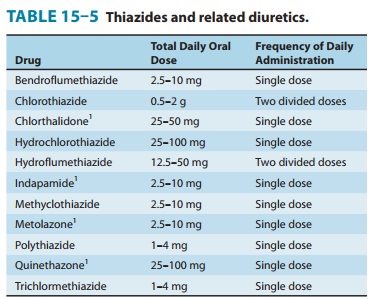
All
thiazides can be administered orally, but there are differ-ences in their
metabolism. Chlorothiazide, the parent of the group, is not very lipid-soluble
and must be given in relatively large doses. It is the only thiazide available
for parenteral adminis-tration. HCTZ is considerably more potent and should be
used in much lower doses (Table 15–5). Chlorthalidone is slowly absorbed and has
a longer duration of action. Although indapamide is excreted primarily by the
biliary system, enough of the active form is cleared by the kidney to exert its
diuretic effect in the DCT.
All
thiazides are secreted by the organic acid secretory system in the proximal
tubule and compete with the secretion of uric acid by that system. As a result,
thiazide use may blunt uric acid secre-tion and elevate serum uric acid level.
Pharmacodynamics
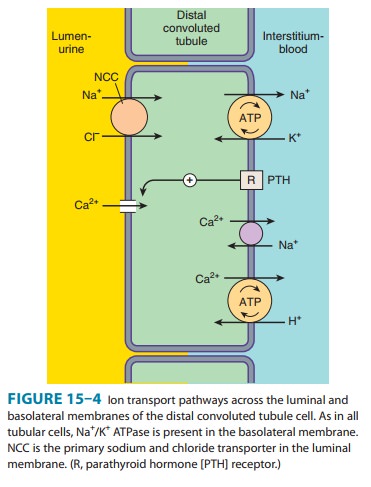
Thiazides
inhibit NaCl reabsorption from the luminal side of epithelial cells in the DCT
by blocking the Na+/Cl− transporter (NCC). In contrast to the situation
in the TAL, in which loop diuretics inhibit Ca2+ reabsorption,
thiazides actually enhance Ca2+ reabsorption. This
enhancement has been postulated to result from effects in both the proximal and
distal convoluted tubules. In the proximal tubule, thiazide-induced volume
deple-tion leads to enhanced Na+ and passive Ca2+ reabsorption. In the
DCT, lowering of intracellular Na+ by thiazide-induced blockade of Na+ entry enhances Na+/Ca2+ exchange in the
basolateral mem-brane (Figure 15–4), and increases overall reabsorption of Ca2+. Although thiazides
rarely cause hypercalcemia as the result of this enhanced reabsorption, they
can unmask hypercalcemia due to other causes (eg, hyperparathyroidism,
carcinoma, sarcoidosis). Thiazides are useful in the treatment of kidney stones
caused by hypercalciuria.
The
action of thiazides depends in part on renal prostaglandin production. As
described for loop diuretics, the actions of thia-zides can also be inhibited
by NSAIDs under certain conditions.
Clinical Indications & Dosage (Table 15–5)
The
major indications for thiazide diuretics are (1) hypertension, heart failure,
(3) nephrolithiasis due to idiopathic hypercalci-uria, and (4) nephrogenic
diabetes insipidus. Use of the thiazides in each of these conditions is
described below in Clinical Pharmacology of Diuretic Agents.
Toxicity
A. Hypokalemic Metabolic Alkalosis and Hyperuricemia
These
toxicities are similar to those observed with loop diuretics (see previous text
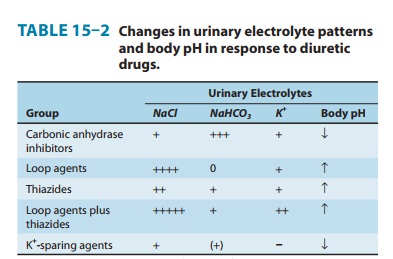
and Table 15–2).
B. Impaired Carbohydrate Tolerance
Hyperglycemia
may occur in patients who are overtly diabetic or who have even mildly abnormal
glucose tolerance tests. The effect is due to both impaired pancreatic release
of insulin and dimin-ished tissue utilization of glucose. Hyperglycemia may be
partially reversible with correction of hypokalemia.
C. Hyperlipidemia
Thiazides
cause a 5–15% increase in total serum cholesterol and low-density lipoproteins
(LDLs). These levels may return toward baseline after prolonged use.
D. Hyponatremia
Hyponatremia
is an important adverse effect of thiazide diuretics. It is caused by a
combination of hypovolemia-induced elevation of ADH, reduction in the diluting
capacity of the kidney, and increased thirst. It can be prevented by reducing
the dose of the drug or limiting water intake.
E. Allergic Reactions
The
thiazides are sulfonamides and share cross-reactivity with other members of
this chemical group. Photosensitivity or gener-alized dermatitis occurs rarely.
Serious allergic reactions are extremely rare but do include hemolytic anemia,
thrombocytope-nia, and acute necrotizing pancreatitis.
F. Other Toxicities
Weakness,
fatigability, and paresthesias similar to those of car-bonic anhydrase
inhibitors may occur. Impotence has been reported but is probably related to
volume depletion.
Contraindications
Excessive
use of any diuretic is dangerous in patients with hepatic cirrhosis, borderline
renal failure, or heart failure (see text that follows).
Related Topics