Chapter: Basic & Clinical Pharmacology : Diuretic Agents
Loop Diuretics
LOOP DIURETICS
Loop
diuretics selectively inhibit NaCl reabsorption in the TAL. Because of the
large NaCl absorptive capacity of this segment and the fact that the diuretic
action of these drugs is not limited by development of acidosis, as is the case
with the carbonic anhydrase inhibitors, loop diuretics are the most efficacious
diuretic agents currently available.
Chemistry
The
two prototypical drugs of this group are furosemide
and ethacrynic acid. The structures
of these diuretics are shown inFigure 15–7. In addition to furosemide, bumetanide and torsemide are sulfonamide loop diuretics.
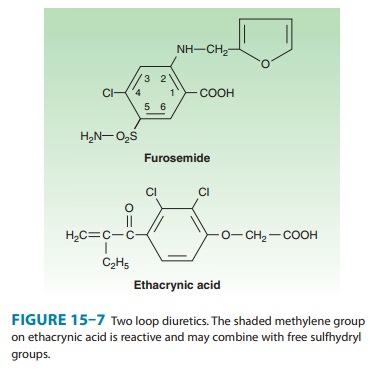
Ethacrynic
acid—not a sulfonamide derivative—is a phenoxy-acetic acid derivative
containing an adjacent ketone and methyl-ene group (Figure 15–7). The methylene
group (shaded in figure) forms an adduct with the free sulfhydryl group of
cysteine. The cysteine adduct appears to be an active form of the drug.
Organic
mercurial diuretics also inhibit
salt transport in the TAL but are no longer used because of their toxicity.
Pharmacokinetics
The
loop diuretics are rapidly absorbed. They are eliminated by the kidney by glomerular
filtration and tubular secretion. Absorption of oral torsemide is more rapid (1
hour) than that of furosemide (2–3 hours) and is nearly as complete as with
intrave-nous administration. The duration of effect for furosemide is usu-ally
2–3 hours. The effect of torsemide lasts 4–6 hours. Half-life
Since loop agents act on the luminal side of the tubule,
their diuretic activity correlates with their secre-tion by the proximal tubule.
Reduction in the secretion of loop diuretics may result from simultaneous
administration of agents such as NSAIDs or probenecid, which compete for weak
acid secretion in the proximal tubule. Metabolites of ethacrynic acid and
furosemide have been identified, but it is not known if they have any diuretic
activity. Torsemide has at least one active metab-olite with a half-life
considerably longer than that of the parent compound.
Pharmacodynamics
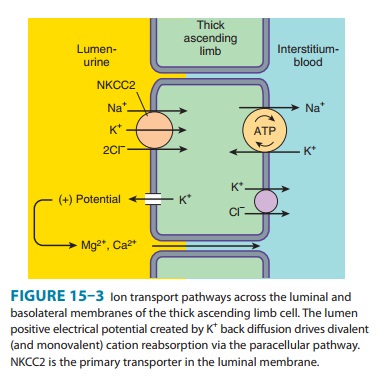
Loop
diuretics inhibit NKCC2, the luminal Na+/K+/2Cl−
trans-porter in the TAL of Henle’s loop. By inhibiting this transporter, the
loop diuretics reduce the reabsorption of NaCl and also diminish the
lumen-positive potential that comes from K+ recy-cling (Figure
15–3). This positive potential normally drives divalent cation reabsorption in
the TAL (Figure 15–3), and by reducing this potential, loop diuretics cause an
increase in Mg2+ and Ca2+ excretion. Prolonged
use can cause significant hypomag-nesemia in some patients. Since vitamin
D–induced intestinal absorption and parathyroid hormone-induced renal
reabsorption of Ca2+ can be increased, loop diuretics do not generally cause hypocalcemia. However, in disorders that
cause hypercalcemia,Ca2+ excretion can be
usefully enhanced by treatment with loop diuretics combined with saline
infusions.
Loop
diuretics have also been shown to induce expression of one of the
cyclooxygenases (COX-2), which participates in the synthesis of prostaglandins
from arachidonic acid. At least one of these prostaglandins, PGE2,
inhibits salt transport in the TAL and thus participates in the renal actions
of loop diuretics. NSAIDs (eg, indomethacin), which blunt cyclooxygenase
activity, can interfere with the actions of loop diuretics by reducing
prostaglandin synthesis in the kidney. This interference is minimal in
otherwise normal subjects but may be significant in patients with nephrotic
syndrome or hepatic cirrhosis.
Loop
agents have direct effects on blood flow through several vascular beds.
Furosemide increases renal blood flow via prosta-glandin actions on kidney
vasculature. Both furosemide and ethacrynic acid have also been shown to reduce
pulmonary con-gestion and left ventricular filling pressures in heart failure
before a measurable increase in urinary output occurs. These effects on
peripheral vascular tone are also due to release of renal prostaglan-dins that
were induced by the diuretics.
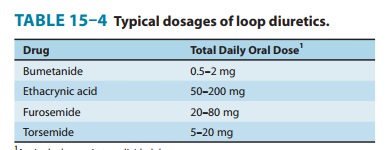
Clinical Indications & Dosage (Table 15–4)
The
most important indications for the use of the loop diuretics include acute pulmonary edema, other edematous
conditions, and acute hypercalcemia.
The use of loop diuretics in these con-ditions is discussed below in Clinical
Pharmacology. Other indica-tions for loop diuretics include hyperkalemia, acute
renal failure, and anion overdose.
A. Hyperkalemia
In
mild hyperkalemia—or after acute management of severe hyperkalemia by other
measures—loop diuretics can significantly enhance urinary excretion of K+. This response is
enhanced by simultaneous NaCl and water administration.
B. Acute Renal Failure
Loop
agents can increase the rate of urine flow and enhance K+ excretion in acute
renal failure. However, they cannot prevent or shorten the duration of renal
failure. If a large pigment load has precipitated acute renal failure (or
threatens to), loop agents may help flush out intratubular casts and ameliorate
intratubular obstruction. On the other hand, loop agents can actually worsen
cast formation in myeloma and light chain nephropathy because increased distal
Cl− concentration enhances secretion of Tamm-Horsfall protein, which
then aggregates with myeloma Bence Jones proteins.
C. Anion Overdose
Loop
diuretics are useful in treating toxic ingestions of bromide, fluoride, and
iodide, which are reabsorbed in the TAL. Saline solu-tion must be administered
to replace urinary losses of Na+ and to provide Cl−, so as to avoid extracellular
fluid volume depletion.
Toxicity
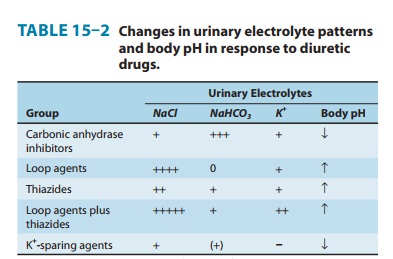
A. Hypokalemic Metabolic Alkalosis
By
inhibiting salt reabsorption in the TAL, loop diuretics increase Na+ delivery to the
collecting duct. Increased delivery leads to increased secretion of K+ and H+ by the duct, causing
hypokalemic metabolic alkalosis (Table 15–2). This toxicity is a function of
the magnitude of the diuresis and can be reversed by K+ replacement and
correction of hypovolemia.
B. Ototoxicity
Loop
diuretics occasionally cause dose-related hearing loss that is usually
reversible. It is most common in patients who have dimin-ished renal function
or who are also receiving other ototoxic agents such as aminoglycoside
antibiotics.
C. Hyperuricemia
Loop
diuretics can cause hyperuricemia and precipitate attacks of gout. This is
caused by hypovolemia-associated enhancement of uric acid reabsorption in the
proximal tubule. It may be prevented by using lower doses to avoid development
of hypovolemia.
D. Hypomagnesemia
Magnesium
depletion is a predictable consequence of the chronic use of loop agents and
occurs most often in patients with dietary magnesium deficiency. It can be
reversed by administration of oral magnesium preparations.
E. Allergic and Other Reactions
All
loop diuretics, with the exception of ethacrynic acid, are sulfonamides.
Therefore, skin rash, eosinophilia, and less often, interstitial nephritis are
occasional adverse effects of these drugs. This toxicity usually resolves
rapidly after drug withdrawal. Allergic reactions are much less common with
ethacrynic acid.
Because
Henle’s loop is indirectly responsible for water reabsorption by the downstream
collecting duct, loop diuretics can cause severe dehydration. Hyponatremia is
less common than with the thiazides , but patients who increase water intake in
response to hypovolemia-induced thirst can become severely hyponatremic with
loop agents. Loop agents can cause hypercalciuria, which can lead to mild
hypocalcemia and secondary hyperparathyroidism. On the other hand, loop agents
can have the opposite effect (hypercalcemia) in volume-depleted patients who
have another—previously occult—cause for hypercalcemia, such as metastatic
breast or squamous cell lung carcinoma.
Contraindications
Furosemide,
bumetanide, and torsemide may exhibit allergic cross-reactivity in patients who
are sensitive to other sulfonamides, but this appears to be very rare.
Overzealous use of any diuretic is dangerous in hepatic cirrhosis, borderline
renal failure, or heart failure.
Related Topics