Chapter: Basic & Clinical Pharmacology : Diuretic Agents
Agents That Alter Water Excretion (Aquaretics)
AGENTS THAT ALTER WATER EXCRETION
(AQUARETICS)
OSMOTIC DIURETICS
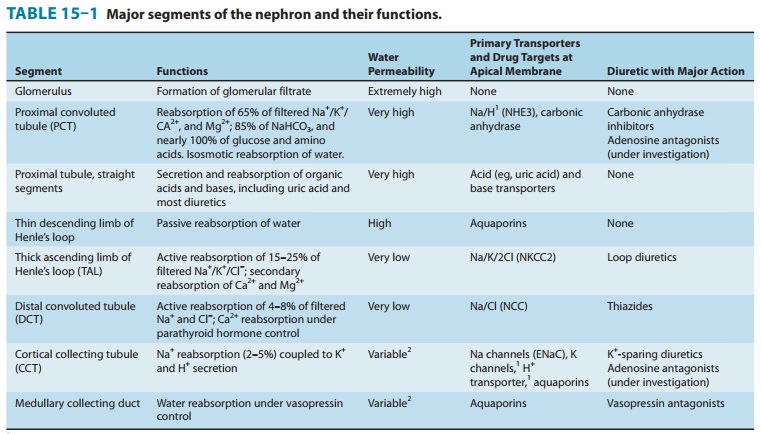
The
proximal tubule and descending limb of Henle’s loop are freely permeable to
water (Table 15–1). Any osmotically active agent that is filtered by the
glomerulus but not reabsorbed causes water to be retained in these segments and
promotes a water diure-sis. Such agents can be used to reduce intracranial
pressure and to promote prompt removal of renal toxins. The prototypic osmotic
diuretic is mannitol. Glucose is not
used clinically as a diuretic but frequently causes osmotic diuresis
(glycosuria) in patients with hyperglycemia.
Pharmacokinetics
Mannitol
is poorly absorbed by the GI tract, and when adminis-tered orally, it causes
osmotic diarrhea rather than diuresis. For systemic effect, mannitol must be
given intravenously. Mannitol is not metabolized and is excreted by glomerular
filtration within 30–60 minutes, without any important tubular reabsorption or
secretion. It must be used cautiously in patients with even mild renal
insufficiency .
Pharmacodynamics
Osmotic
diuretics have their major effect in the proximal tubule and the descending
limb of Henle’s loop. Through osmotic effects, they also oppose the action of
ADH in the collecting tubule. The presence of a nonreabsorbable solute such as
mannitol prevents the normal absorption of water by interposing a
countervailing osmotic force. As a result, urine volume increases. The increase
in urine flow rate decreases the contact time between fluid and the tubular
epithelium, thus reducing Na+ as well as water reabsorp-tion. The resulting natriuresis is of
lesser magnitude than the water diuresis, leading eventually to excessive water
loss and hypernatremia.
Clinical Indications & Dosage
A. Increase of Urine Volume
Osmotic
diuretics are used to increase water excretion in prefer-ence to sodium
excretion. This effect can be useful when avid Na+ retention limits the
response to conventional agents. It can be used to maintain urine volume and to
prevent anuria that might other-wise result from presentation of large pigment
loads to the kidney (eg, from hemolysis or rhabdomyolysis). Some oliguric
patients do not respond to osmotic diuretics. Therefore, a test dose of
mannitol (12.5 g intravenously) should be given before starting a continu-ous
infusion. Mannitol should not be continued unless there is an increase in urine
flow rate to more than 50 mL/h during the 3 hours after the test dose. Mannitol
(12.5–25 g intravenously) can be repeated every 1–2 hours to maintain urine
flow rate greater than 100 mL/h. Prolonged use of mannitol is not advised.
B. Reduction of Intracranial and Intraocular Pressure
Osmotic
diuretics alter Starling forces so that water leaves cells and reduces
intracellular volume. This effect is used to reduce intrac-ranial pressure in
neurologic conditions and to reduce intraocular pressure before ophthalmologic
procedures. A dose of 1–2 g/kg mannitol is administered intravenously.
Intracranial pressure, which must be monitored, should fall in 60–90 minutes.
Toxicity
A. Extracellular Volume Expansion
Mannitol
is rapidly distributed in the extracellular compartment and extracts water from
cells. Prior to the diuresis, this leads to expansion of the extracellular
volume and hyponatremia. This effect can complicate heart failure and may
produce florid pulmo-nary edema. Headache, nausea, and vomiting are commonly
observed in patients treated with osmotic diuretics.
B. Dehydration, Hyperkalemia, and Hypernatremia
Excessive
use of mannitol without adequate water replacement can ultimately lead to
severe dehydration, free water losses, and hyper-natremia. As water is
extracted from cells, intracellular K+ concen-tration rises,
leading to cellular losses and hyperkalemia. These complications can be avoided
by careful attention to serum ion composition and fluid balance.
C. Hyponatremia
When
used in patients with severe renal impairment, parenterally administered mannitol
cannot be excreted and is retained intrave-nously. This causes osmotic
extraction of water from cells, leading to hyponatremia.
ANTIDIURETIC HORMONE (ADH, VASOPRESSIN) AGONISTS
Vasopressin and
desmopressin are used in the treatment of cen-tral diabetes insipidus.
Their renal action appears to be mediated primarily via V2 ADH
recep-tors, although V1a receptors may also be involved.
ANTIDIURETIC HORMONE ANTAGONISTS
A variety of medical conditions, including congestive heart failure (CHF) and the syndrome of inappropriate ADH secretion (SIADH), cause water retention as a result of excessive ADH secretion. Patients with CHF who are on diuretics frequently develop hyponatremia secondary to excessive ADH secretion.Dangerous hyponatremia can result.
Until
recently, two nonselective agents, lithium and demeclocycline, were used for
their well-known interfer-ence with ADH activity. The mechanism for this
interference has not been completely determined for either of these agents.
Demeclocycline is used more often than lithium because of the many side effects
of lithium administration. However, demeclocy-cline is now being rapidly
replaced by several specific ADH recep-tor antagonists (vaptans), which have
yielded encouraging clinical results.
There
are three known vasopressin receptors,V1a, V1b, and V2.
V1 receptors are expressed in the vasculature and CNS, while V2
recep-tors are expressed specifically in the kidney. Conivaptan (currently available only for intravenous use) exhibits
activity against both V1a and V2 receptors . The oral
agentstolvaptan, lixivaptan, and
satavaptan are selectively active against the V2 receptor.
Lixivaptan and satavaptan are still under clinical investigation, but
tolvaptan, which recently received Food and Drug Administration approval, is
very effective in treatment of hyponatremia and as an adjunct to standard
diuretic therapy in patients with CHF.
Pharmacokinetics
The
half-life of conivaptan and demeclocycline is 5–10 hours, while that of
tolvaptan is 12–24 hours.
Pharmacodynamics
Antidiuretic
hormone antagonists inhibit the effects of ADH in the collecting tubule.
Conivaptan and tolvaptan are direct ADH receptor antagonists, while both
lithium and demeclocycline reduce ADH-induced cAMP by mechanisms that are not
yet com-pletely clarified.
Clinical Indications & Dosage
A. Syndrome of Inappropriate ADH Secretion
Antidiuretic
hormone antagonists are used to manage SIADH when water restriction has failed
to correct the abnormality. This generally occurs in the outpatient setting,
where water restriction cannot be enforced, but can occur in the hospital when
large quantities of intravenous fluid are needed for other purposes.
Demeclocycline (600–1200 mg/d) or tolvaptan (15–60 mg/d) can be used for SIADH.
Appropriate plasma levels of demeclocycline (2 mcg/mL) should be maintained by
monitoring, but tolvaptan levels are not routinely monitored. Unlike
demeclocycline or tolvaptan, conivaptan is administered intravenously and is
not suitable for chronic use in outpatients. Lixivaptan and satavaptan may also
soon be available for oral use.
B. Other Causes of Elevated Antidiuretic Hormone
Antidiuretic
hormone is also elevated in response to diminished effec-tive circulating blood
volume, as often occurs in heart failure. When treatment by volume replacement
is not desirable, hyponatremia may result. As for SIADH, water restriction is
often the treatment of choice. In patients with heart failure, this approach is
often unsuccess-ful in view of increased thirst and the large number of oral
medica-tions being used. For patients with heart failure, intravenous
conivaptan may be particularly useful because it has been found that the
blockade of V1a receptors by this drug leads to decreased
periph-eral vascular resistance and increased cardiac output.
Toxicity
A. Nephrogenic Diabetes Insipidus
If
serum Na+ is not monitored closely, any ADH antagonist can cause severe
hypernatremia and nephrogenic diabetes insipidus. If lithium is being used for
a psychiatric disorder, nephrogenic dia-betes insipidus can be treated with a
thiazide diuretic or amiloride (see Diabetes Insipidus, below).
B. Renal Failure
Both
lithium and demeclocycline have been reported to cause acute renal failure.
Long-term lithium therapy may also cause chronic interstitial nephritis.
C. Other
Dry
mouth and thirst are common with many of these drugs. Tolvaptan may cause
hypotension. Demeclocycline should be avoided in patients with liver
disease and in children younger than 12
years.
Related Topics