Chapter: Basic Radiology : Imaging of the Heart and Great Vessels
Technique Selection
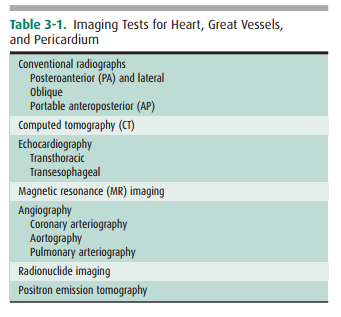
TECHNIQUE
SELECTION
There is a wide array of imaging
tests that can be used to eval-uate the cardiovascular system (see Table 3-1).
After a thor-ough history and physical examination, the initial screening study
should always be a chest radiograph. Ideally, the PA and lateral views should
be obtained with maximum inspiration. This study gives important information
about the cardiac contour and the status of the lungs, and it is a good
examina-tion for excluding disorders that would require immediate treatment,
such as pneumothorax. Furthermore, evaluation of the chest radiograph can often
lead to a specific diagnosis and treatment, such as in congestive heart
failure, or can help determine the need for another imaging study. Depending on
the history and physical examination find-ings, echocardiography, nuclear
cardiac imaging, CT, MR, or conventional coronary angiography may follow.
Echocardiog-raphy is a good screening test to assess cardiac and great-vessel
valvular motion and structural abnormalities, cardiac cham-ber morphology, and
flow. Angiography delineates the struc-tural status of the coronary arteries
and can give information on blood flow through the cardiac chambers, valves,
and prox-imal great vessels, mainly in patients with suspected
athero-sclerosis. It is also used to guide interventions such as stent
placement in the coronary arteries. Because of its inherent risks, coronary
arteriography is usually reserved for patients with signs and symptoms of
myocardial ischemia or infarction on the basis either of history or of results
of electrocardiogra-phy, echocardiography, or radionuclide myocardial imaging.
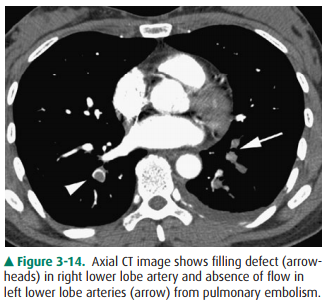
In patients with suspected
pulmonary emboli, helical CT is the most appropriate test in the setting of an
abnormal chest x-ray (Figure 3-14). The ventilation-perfusion (V/Q) scan can be
performed if the chest radiograph is normal and is also the preferred
examination in young females because of the radiation dose to the breast by CT.
Both of these tests can confirm the clinically suspected diagnosis of pulmonary
em-bolic disease and often provide a useful “map” of the most suspicious
regions of the lung for the angiographer if an an-giogram is required for the
definitive diagnosis of pulmonary embolism. CT can also detect important
alternative diag-noses not detected by either V/Q scan or pulmonary
angiog-raphy. More frequently, patients with atypical chest pain are being
referred for the triple rule-out examination. This test is not appropriate for
patients with clear signs or symptoms of myocardial ischemia and should be
reserved for intermediate-to low-risk patients with a nondiagnostic ECG and
negative first set of troponins.
Echocardiography, MR imaging, or
CT or cardiac angiog-raphy may be selected for patients with suspected
congenital heart disease. The advantages of MR imaging in this setting is that
it is noninvasive, generally needs no contrast material ad-ministration, and
uses no ionizing radiation, an important consideration in the pediatric
patient. For these reasons, MR imaging has become the preferred imaging test in
the pediatric population. As dose reduction techniques have improved, the use
of CT for congenital heart disease has also increased.
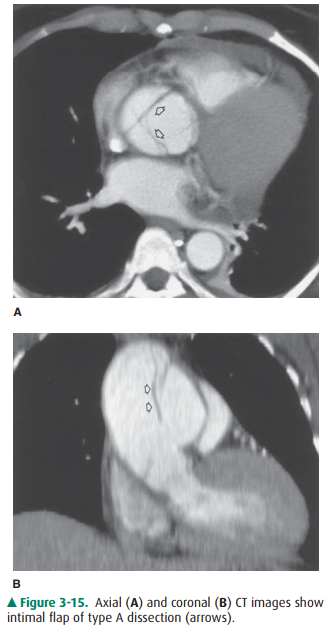
Suspected aortic dissection (either
atherosclerotic or traumatic in origin) can be evaluated by helical CT, TEE,
aortography, or MR imaging. Helical CT is the imaging modality of choice for
acute dissection because of its accu-racy and availability (Figure 3-15). With
multislice technol-ogy, CT angiography can provide images in multiple planes to
show the relation of the dissection to key branch vessels. TEE has the
advantages of being quick and noninvasive, and the examination can be performed
expediently at the bed-side. MR imaging is noninvasive, uses no ionizing
radiation, is less operator-dependent, and can be performed in multi-ple
planes. It is limited by availability and imaging time and because it cannot be
used in patients with certain implanted devices, particularly pacemakers. Angiography
has mostly been relegated to minimally invasive treatments such as stent-graft
placement. Because survival rates often depend on early surgical intervention,
availability and timeliness of the examinations is important.
In patients whose chest radiographs
suggest intrinsic pul-monary or mediastinal processes, a standard chest CT is
cur-rently the preferred modality. The use of contrast depends on the
indication, the preference of the radiologist, and any pos-sible
contraindications to administration of intravenous con-trast for individual
patients.
Finally, regardless of the
situation, it is reasonable for the clinician and radiologist to decide
together which imaging tests are most appropriate. In many instances, the
choice of the next most efficacious and least costly imaging examina-tion is
not always clear-cut. In fact, in some circumstances, it is not necessary to
perform another test because of the lim-ited potential yield from the
examination or because there is no adequate therapy for the suspected
abnormality. It is hoped that future recommendations for test selection will be
determined by well-designed prospective unbiased outcome studies comparing all
of these modalities in various clinical scenarios. In the meantime, a
commonsense approach, tak-ing into consideration the history and physical
examination findings, the information gleaned from the conventional
ra-diograph, and the potential yield from the array of other available imaging
tests, is the most appropriate. In all in-stances, communication between the
clinician and radiolo-gist is critical for the best patient care.
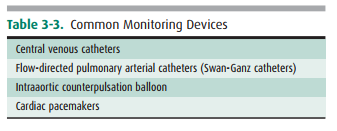
Monitoring Devices
In clinical hospital practice,
particularly in the ICU setting, a variety of catheters and tubes are used to
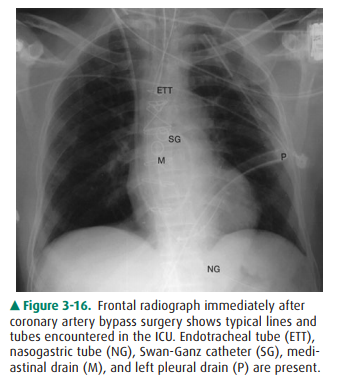
monitor various parameters in patients (Figure 3-16). The student should be
familiar with the normal routes and positions of these de-vices, as well as
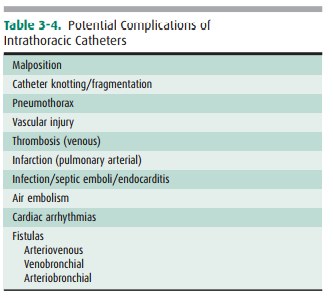
inappropriate positions and complications. Table 3-3 lists the most common
monitoring devices.
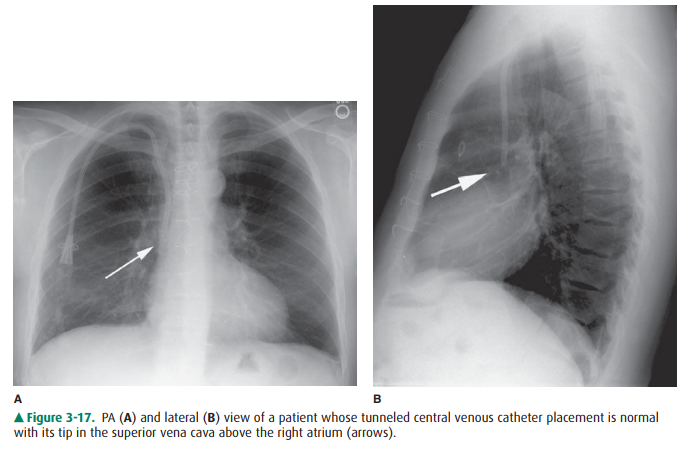
The basic venous anatomy of the
upper mediastinum should be reviewed and kept in mind when evaluating catheter
placement. The most common routes of catheter insertion in the chest include
the internal jugular and subclavian veins. Ra-diographs obtained after
insertion show the catheter following the course of either the internal jugular
or subclavian vein and passing through the brachiocephalic vein. It then curves
gently downward to terminate in the superior vena cava proximal to the right
atrium (Figure 3-17). One normal variation of ve-nous anatomy is the persistent
left superior vena cava. In this situation the catheter descends down the left
mediastinum ter-minating in the left SVC. The left SVC ultimately drains into
the coronary sinus, which then enters the right atrium.
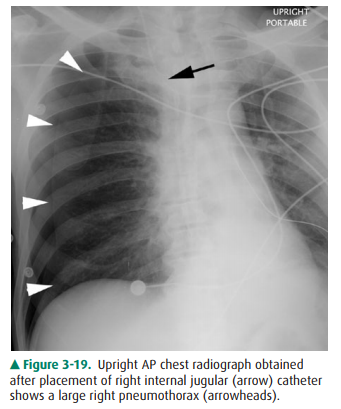
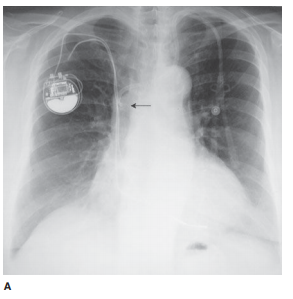
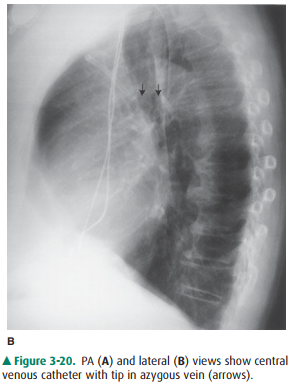
Intrathoracic central venous
catheters are used mainly for monitoring central venous pressure (CVP),
maintaining proper nutrition, delivering medication, and hemodialysis. It is
standard practice to request a chest radiograph after catheter placement to
verify its location (Figure 3-18) and to check for potential complications,
such as pneumothorax (Figure 3-19) or hemothorax. Measurement of CVP is
opti-mally obtained when the tip of the catheter is proximal to the right
atrium and distal to the most proximal valves of the large veins. A catheter
tip proximal to the veins gives an inaccuratereading of CVP, and a tip too close
to the right atrium may cause arrhythmias from irritation of the right atrial
my-ocardium. The reason for catheter insertion is critical for iden-tifying its
appropriate position. If it has been placed just for fluids and/or medications,
a termination in the brachio-cephalic vein is satisfactory. Conversely, a
plasmapheresis catheter should never be located in the right atrium because of
the risk of complications. More frequently, central venous catheters are being
placed centrally via a peripheral vein. Thesecatheters have minimal risk, can
remain in place for longer pe-riods of time without being exchanged, and are
primarily used for the delivery of fluids and long-term antibiotics.
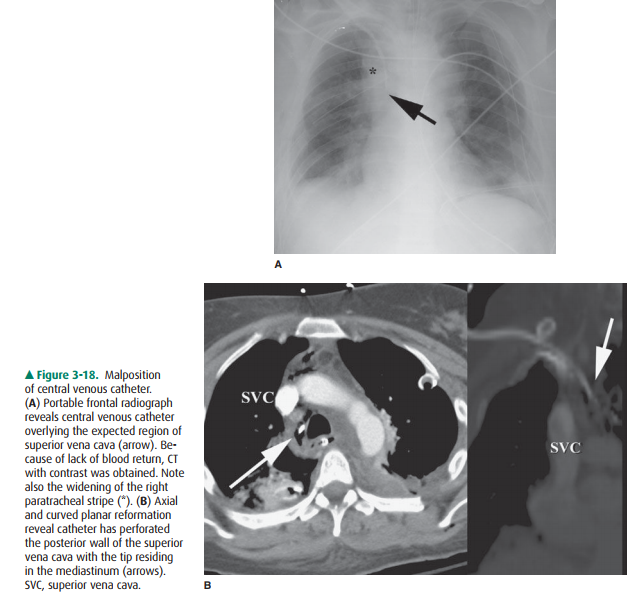
The major potential complications
from catheter place-ment are outlined in Table 3-4. A malpositioned central
ve-nous catheter may result in inaccurate CVP measurement, thrombosis, catheter
knotting, and infusion of substances into the mediastinum or pleura. Catheter
tips against the wall of the SVC may erode into the mediastinum or may
extendretrograde into tributary veins, particularly the azygous vein (Figure
3-20).
Flow-directed arterial catheters
are also regularly used in cardiac and ICU patients to monitor cardiac output.
The most common flow-directed catheter is the Swan-Ganz (SG) catheter (see
Figure 3-16). It is usually inserted percutaneouslyinto the left or right
subclavian vein and threaded through the brachiocephalic vein, superior vena
cava, right atrium, tricus-pid valve, right ventricle, pulmonic valve, and
directed out into the main pulmonary artery. Usually terminating in the right
or left pulmonary arteries, the SG tip should be distal to the pulmonary valve
and proximal to the smaller pulmonary ar-terial vessels so it will not cause
occlusion and, potentially, thrombosis. A simple rule of thumb is that the
catheter should not extend past the mediastinal borders. It may then be
intermittently “wedged” into a distal pulmonary artery branch to obtain a
pulmonary capillary wedge pressure.
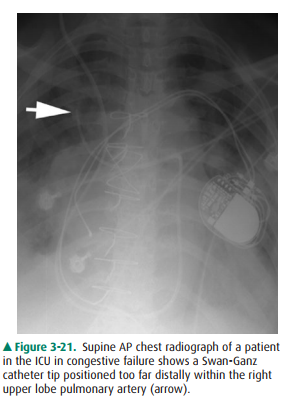
Complications of SG catheter placement are similar to those with other central venous catheters. The tip may be po-sitioned in a number of inappropriate vessels or locations, and a chest radiograph should be obtained after catheter in-sertion to confirm its position (Figure 3-21). Introduction of any catheter into the subclavian vein, because of its close proximity to the lung apex, can cause pneumothorax (see Figure 3-19). A catheter tip position in the right ventricle can lead to ventricular arrhythmias, and leaving the catheter tip too distal may result in a pulmonary artery pseudoaneurysm or pulmonary infarct.
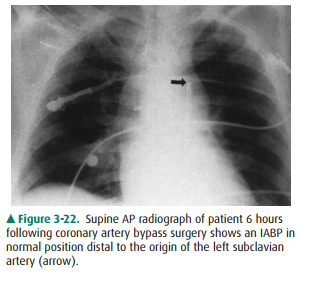
An intraaortic counterpulsation
balloon pump (IABP) is occasionally used in patients with cardiogenic shock.
This catheter measures approximately 26 cm in length and is sur-rounded by a
balloon, which inflates with helium or carbon dioxide gas during diastole and
deflates during systole. Defla-tion during systole decreases afterload and
results in dimin- ished left ventricular work and oxygen requirements, while
the inflation of the balloon during diastole increases cardiac pressure to help
ensure adequate perfusion of the coronary arteries. The catheter, introduced
percutaneously into the thoracic aorta via the common femoral artery or placed
into the ascending aorta at the time of surgery, should be posi-tioned so that
its tip is just distal to the origin of the left sub-clavian artery. The tip of
the catheter has a small radiopaque marker so that this position can be
ascertained on the chest radiograph (Figure 3-22). The major complications of
the IAPB result from positioning of its tip proximal to the left subclavian
artery, which may cause occlusion of the left sub-clavian vessel orifice,
cerebral artery embolization, or aortic tear. If positioned too low, the
balloon may occlude the celiac, superior mesenteric, and renal arteries.
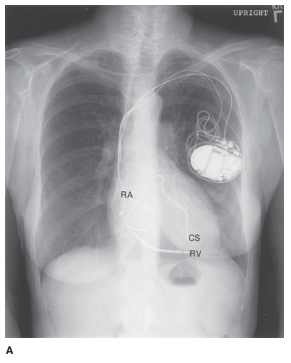
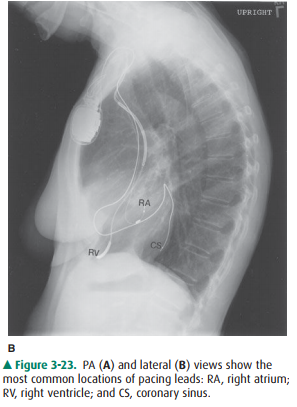
Unipolar or bipolar pacemakers
are most common and are usually implanted in the chest wall with leads inserted
into the subclavian vein. The unipolar pacemaker tip is normally situated at
the apex of the right ventricle. The bipolar pacemaker has a proximal lead that
terminates in the right atrium and a distal lead that terminates within the
right ventricle (similar to the unipolar pacemaker posi-tion). Biventricular
pacemakers have a third lead present in the coronary sinus, appearing superior
to the right ventric-ular lead (Figure 3-23). Its posterior position can be
con-firmed on the lateral view. Pacemakers that also have the ability to act as
defibrillators have larger leads with a coil spring appearance. Leads are
usually placed from a transve-nous approach, although in certain circumstances
they can be placed directly on the epicardium through the chest wall. The
purpose of the chest radiograph after the pace-maker insertion is to document
the appropriate placement of these leads, to check for complications from placement,
and to establish a baseline examination to compare with future chest
radiographs.
Related Topics