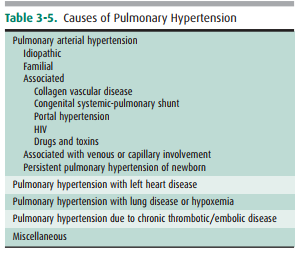
Chapter: Basic Radiology : Imaging of the Heart and Great Vessels
Exercise : Alterations In Cardiac Contour
EXERCISE 3-2. ALTERATIONS IN CARDIAC CONTOUR
3-6. In Case 3-6 (Figure 3-32), the most likely cause of the radiographic abnormality is
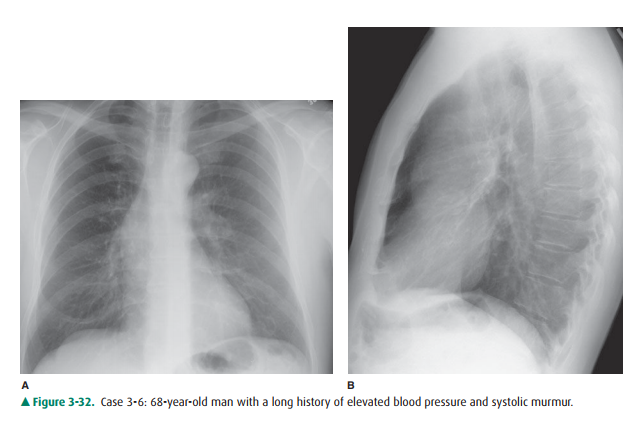
A. syphilis.
B. cystic medial necrosis.
C. aortic stenosis.
D. congenital heart disease.
E. drug abuse.
3-7. In Case 3-7 (Figure 3-33), the abnormality is due to
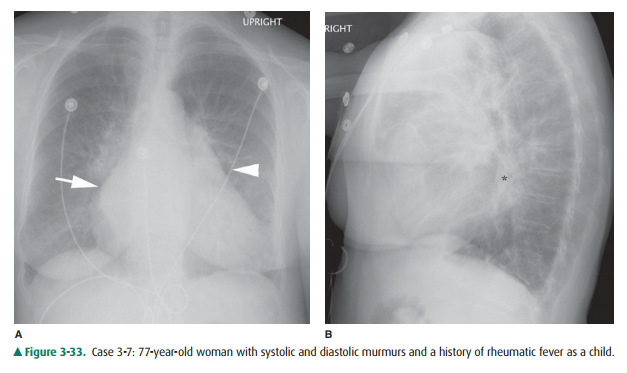
A. mitral valve disease.
B. left ventricular hypertrophy.
C. pulmonic stenosis.
D. right atrial enlargement.
E. mediastinal mass.
3-8. In Case 3-8 (Figure 3-34), what is the cardiac contour abnormality?
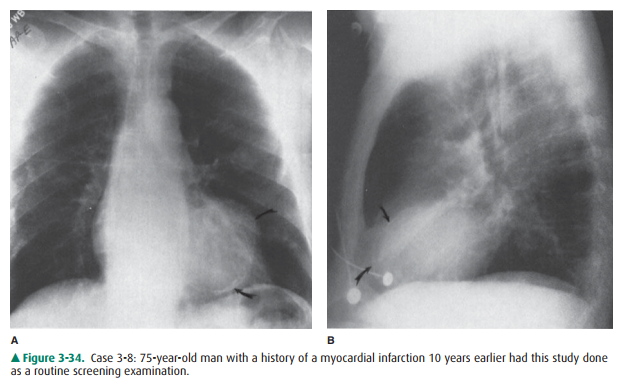
A. Left atrial enlargement
B. Left ventricular enlargement
C. Right atrial enlargement
D. Left ventricular aneurysm
E. Right ventricular aneurysm
3-9. The diagnosis in Case 3-9 (Figure 3-35) is
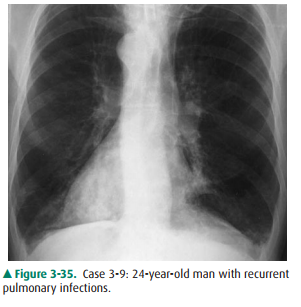
A. situs inversus.
B. dextrocardia.
C. technical aberration.
D. tetralogy of Fallot.
E. pulmonary atresia.
3-10. The configuration of the heart in Case 3-10 (Figure3-36) has been called the
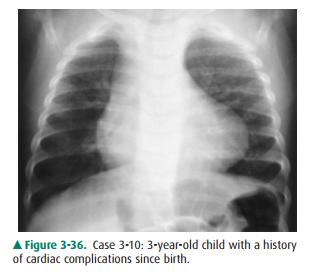
A. boot-shaped heart.
B. third mogul of the heart.
C. snowman appearance.
D. double contour sign.
E. water-bottle heart.
Radiographic Findings
3-6. In this case (Figure 3-32), the classical findings of en-largement of the left ventricle, characteristic of left ventricular hypertrophy, are seen on both the PA and the lateral radiograph as well as deviation of the as-cending aorta contour to the right. This pattern is often the result of long-standing aortic stenosis (C is the correct answer to Question 3-6).
3-7. In this case (Figure 3-33), a double density to the right side of the heart is seen on the PA radiograph (arrow). There is also an enlarged left atrial appendage (arrow-head). The lateral radiograph shows enlargement of the left atrial shadow, the superior and posterior re-gion of the cardiac contour (*), and posterior displace-ment of the left main bronchus and enlargement of the right ventricle (A is the correct answer to Question 3-7). Along with increased pulmonary vascularity, the constellation of findings is characteristic of left atrial enlargement due to mitral valve insufficiency.
3-8. The PA and lateral radiographs in this case (Figure 3-34) show an enlargement of the left ventricular contour with a focal bulge containing calcification within its wall (arrows). The lateral radiograph con-firms the calcification (curved arrows). Given the his-tory of myocardial infarction 10 years earlier, the most likely diagnosis is a left ventricular aneurysm (D is the correct answer to Question 3-8).
3-9. The patient in this case (Figure 3-35) shows the apex of the heart to be on the right side of the chest and the descending aorta to be in its correct position on the left. These findings are diagnostic of dextrocardia, which in this case is secondary to Kartagener syn-drome (B is the correct answer to Question 3-9).
3-10. In this case (Figure 3-36), tetralogy of Fallot, the apex of the left ventricle is elevated by right ventricular hy-pertrophy. These findings are sometimes referred to as a boot-shaped heart (A is the correct answer to Question 3-10).
Discussion
Left atrial enlargement (LAE), as shown in Case 3-7 (Figure 3-33), occurs mainly with left-sided obstructive lesions such as mitral stenosis or mitral regurgitation, often the result of rheu-matic heart disease. The major sign of LAE on the PA view is a double density centrally caused by the dilated left atrium ex-tending to the right of the spine projected behind the right atrium (Figure 3-33A, arrow). Another sign of LAE is enlarge-ment of the left atrial appendage. The left atrial appendage is immediately adjacent and inferior to the left main bronchus.
When enlarged, there is an extra bump along the left heart bor-der, the so-called third mogul of the left cardiac border (Figure 3-33A, arrowhead). LAE also causes a separation and widening of the carinal angle that can be seen on the PA chest radi-ograph, although this is a late sign of LAE. The carinal angle normally measures between 60 and 120 degrees. Widening of this angle may occasionally be caused by subcarinal adenopa-thy and therefore should be correlated with other signs of LAE.
The left atrium makes up the posterior cardiac shadow just above the left ventricle (LA in Figure 3-1). Left atrial en-largement is recognized on the lateral film by enlargement and posterior displacement of the left atrial shadow (Figure 3-33B, *). As further enlargement occurs, the left atrium dis-places the left main and left lower lobe bronchus posteriorly. Ultimately the elevated left heart pressures can be transmit-ted back across the pulmonary circulation, leading to pul-monary arterial hypertension and subsequent right heart enlargement (see later discussion).
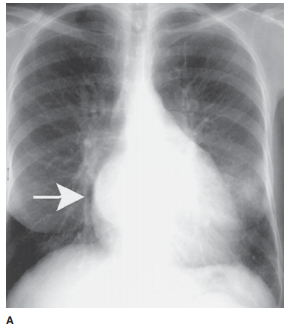
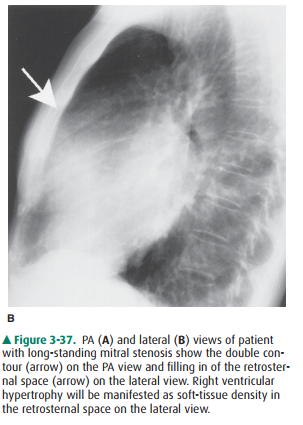
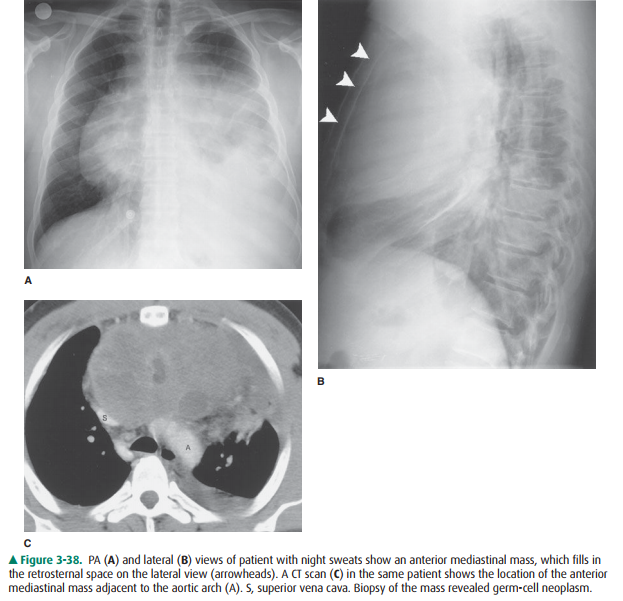
Right ventricular enlargement (RVE) or hypertrophy (RVH) results most commonly from right-sided heart failure from a variety of disorders resulting in pulmonary hyperten-sion (Table 3-5). In this cardiac contour abnormality there is an increase in the soft-tissue density within the retrosternal clear space that is best seen on the lateral radiograph (Figure 3-37). On the PA film, uplifting of the cardiac apex may be also seen. Anterior mediastinal masses may also cause retrosternal soft tis-sue density and should be included in the differential diagnosis (Figure 3-38); however, the majority of anterior mediastinal masses fill the RSS from superior to inferior and may not ob-scure right sided cardiac structures. When the cause is not clear from the conventional radiograph, CT is the next most appro-priate test to differentiate between these two considerations.
Cardiac aneurysms, as shown in the patient in Case 3-8 (Figure 3-34), are almost always the sequelae of myocardialinfarction. There are two types of cardiac aneurysms: true and false aneurysms. True aneurysms most frequently occur at the cardiac apex and contain all three layers of myocardium. False aneurysms or pseudoaneurysms occur with disruption of the endocardium, with dissection of blood into the cardiac wall. Pseudoaneurysms, therefore, are not bound by all three layers of the heart wall. Pseudoaneurysms most frequently occur along the free walls of the heart (inferior and lateral walls). Aneurysms are usually diagnosed on the PA chest radiographas localized soft-tissue outpouchings or irregularities at the apical or anterolateral segments of the left ventricular cardiac contour. A linear rim of dystrophic calcification may develop within the nonviable myocardium after the infarction. With echocardiography, aneurysms show paradoxical enlargement during systole. Because there is stasis of blood in the aneurysm, blood clots can develop and may be a source of dis-tal systemic arterial emboli. Echocardiography, CT, and MR imaging can all be used to make the diagnosis of cardiac aneurysm and distinguish between true and false aneurysms. The distinction is important because false aneurysms are at higher risk for rupture and require surgical repair.
Dextrocardia, as shown in Case 3-9 (Figure 3-35), is usu-ally recognized easily on the PA chest radiograph. However, this finding may be overlooked if the left and right designa-tions on the film are marked incorrectly or are misinter-preted. In most cases of dextrocardia, the aorta descends on the left side and the patient is asymptomatic. If the aorta de-scends on the right side, a number of other abnormalities should be considered. The references provide more in-depth discussion of this topic.
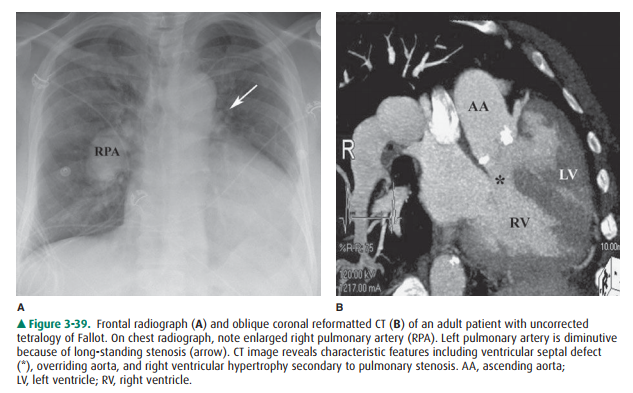
The boot shape of the cardiac shadow in Case 3-10 (Fig-ure 3-36) is secondary to tetralogy of Fallot. The four com-ponents of this congenital cardiac anomaly are an overriding aorta, ventricular septal defect, pulmonic stenosis, and right ventricular hypertrophy. It is the right heart enlargement that results in the upturned cardiac apex. The degree of shunt and pulmonary stenosis dictate the presentation. In cases where the stenosis is severe, infants are cyanotic and there is gener-alized decrease in pulmonary vasculature. If the pulmonary stenosis and degree of left-to-right shunt is mild, the abnor-mality may not manifest itself until childhood (Figure 3-39).
Related Topics