Chapter: Basic Radiology : Imaging of the Heart and Great Vessels
Exercise: Pulmonary Vascularity
EXERCISE 3-3.
PULMONARY VASCULARITY
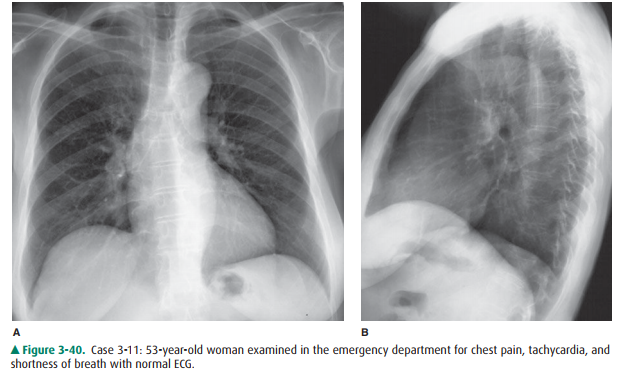
3-11. The most likely
cause of the patient’s symptoms in Case 3-11 (Figure 3-40) is
A.
pneumonia.
B.
pulmonary edema.
C.
interstitial lung disease.
D.
panic attack.
E.
pneumothorax.
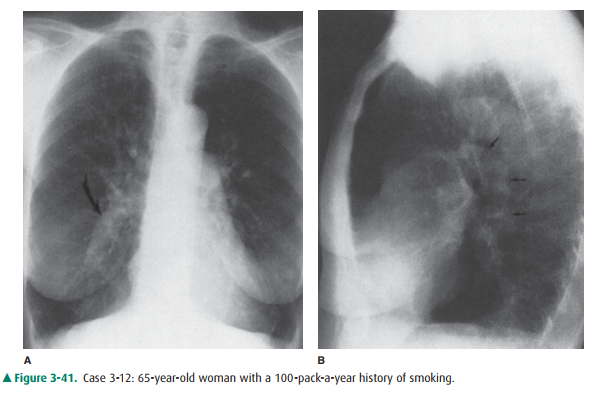
3-12. The curved arrow in
Case 3-12 (Figure 3-41A) is directed to the
A.
right atrium.
B.
ascending aorta.
C.
right descending pulmonary artery.
D.
main pulmonary artery.
E.
pneumonia.
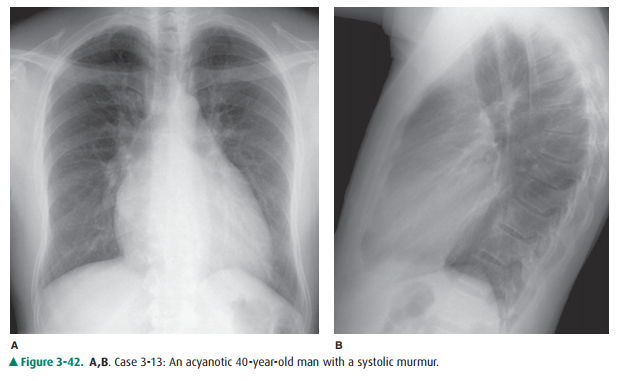
3-13. The most likely
diagnosis in Case 3-13 (Figure 3-42) is
A.
aortic stenosis.
B.
pulmonic stenosis.
C.
VSD.
D.
pulmonary edema.
E.
normal chest radiograph.
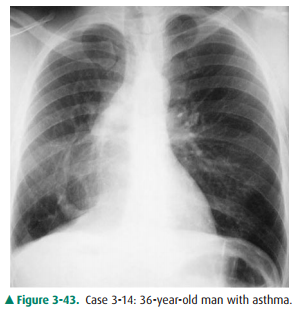
3-14. The appearance of the pulmonary vasculature indicates
that the diagnosis in Case 3-14 (Figure 3-43) isenlarged atrial appendage.
A.
partial anomalous pulmonary venous return.
B.
right ventricular hypertrophy.
C.
left atrial enlargement.
D.
pulmonary arteriovenous malformation.
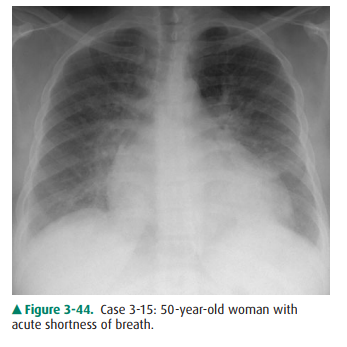
3-15. The most likely
etiology of the radiographic findings in Case 3-15 (Figure 3-44) is
A.
cardiac failure with pulmonary edema.
B.
pulmonic stenosis with pneumonia.
C.
pulmonary embolism.
D.
pneumomediastinum.
E.
pneumothorax.
Radiologic Findings
3-11. In this case
(Figure 3-40), the chest radiograph was normal in a 53-year-old woman seen in
the emer-gency department for left-sided chest pain. The elec-trocardiogram was
also normal, and there was no obvious cause for the patient’s pain. (D is the
correct answer to Question 3-11). Note the well-defined pul-monary vessels in
the perihilar region and normal branching of these vessels into the lungs.
There is a gradient of pulmonary vascular markings from the bases to the apices
on an upright radiograph due to the increased perfusion to the lower lobes. No
pulmonary parenchymal abnormalities are present to support the other diagnoses.
It should be noted that the chest radiograph is often normal in myocardial
infarction, and a normal chest x-ray does not exclude intrinsic cardiac disease
per se.
3-12. This case (Figure
3-41) is an example of chronic obstructive pulmonary disease. The large central
pulmonary arteries indicate pulmonary arterial hypertension. The curved arrow
in Figure 3-41A identifies the enlarged right descending pulmonary artery (C is
the correct answer to Question 3-12). The generalized proximal pulmonary artery
enlargement is confirmed on the lateral radiograph by the large left pulmonary
artery (arrows in Figure 3-41B). Note the attenuation of vessels in the
periphery of the lungs. This constellation of findings is typical of
em-physema. There are also large bullae, which result in an absence of
pulmonary vessels and hyperlucency of the lungs.
3-13. This case (Figure
3-42) shows increased pulmonary vascularity in a 40-year-old patient with VSD
(C is the correct answer to Question 3-13). Note the large central pulmonary
arteries, the increased linear opac-ities radiating out into the lungs, and the
relatively uniform distribution of the pulmonary vascular shadows. In
individuals with long-standing intracar-diac shunts and pulmonary hypertension,
the pul-monary arterial resistance may exceed systemic pressures, resulting in
Eisenmenger’s physiology, a re-versal of an intracardiac shunt from L R to R L.
In these individuals, the central
pulmonary arteries are quite large, but the peripheral pulmonary arteries are
markedly attenuated.
3-14. This case (Figure
3-43) shows the characteristic appearance of venolobar (scimitar) syndrome (B
is the correct answer to Question 3-14). The scimitar vein is the result of
partial anomalous pulmonary venous return.
3-15. This case (Figure
3-44) is an example of a pulmonary edema due to fluid overload and congestive
heart failure (A is the correct answer to Question 3-15). Note the increased
size of the cardiac silhouette, the ill-defined reticular perihilar air-space
opacities, the enlargement of the vascular pedicle, and the redistri-bution of
blood flow to the upper lung zones.
Discussion
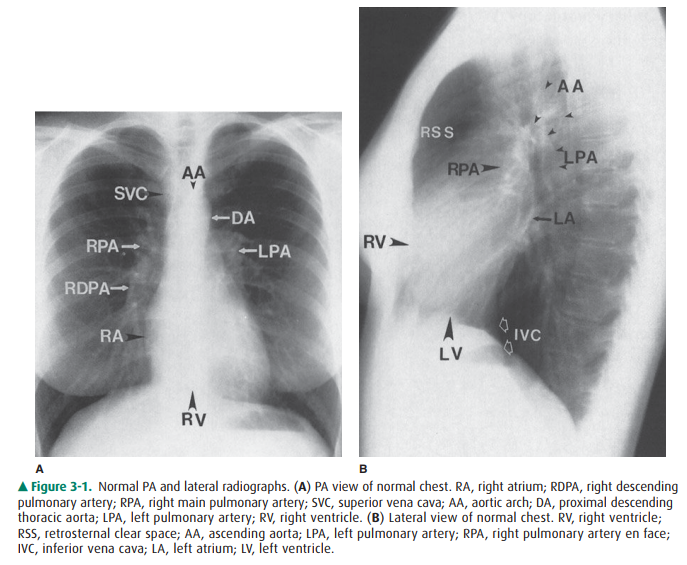
The main pulmonary arteries are
large, the lobar arteries smaller, and each branching segment becomes
progres-sively smaller. As the vasculature tree ramifies, the arteries are
closely related to the adjacent bronchus and are ap-proximately the same size.
On the chest radiograph, this pattern is manifest by linear opacities or
shadows that are much more prominent in the central portion of the chest and
gradually become less prominent toward the periphery of the lung, as in the
normal person in Case 3-11. The right descending pulmonary artery is one
important landmark on the PA chest film (see Figure 3-1). In the normal chest,
the lateral border of the RDPA is usually well demarcated, and the artery
usually measures less than 15 mm in its widest diameter.
Enlargement of the pulmonary
vessels is caused by a vari-ety of abnormalities (see Table 3-5). Chronic
obstructive pul-monary disease, with resultant pulmonary hypertension, is the
most common cause of pulmonary arterial hypertension and is shown in the
patient in Case 3-12 (Figure 3-41).
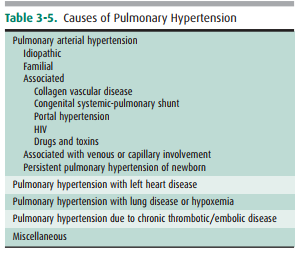
Intracardiac shunts that result
in increased pulmonary ar-terial flow can also enlarge the pulmonary vascular
system. The most common lesions causing increased vascularity without cyanosis
are ASD, VSD, and patent ductus arteriosus (PDA). Case 3-13 (Figure 3-42) is an
example of a VSD with increased vascularity. The main cardiac lesions with
cyanosis and increased pulmonary vascularity are transposition of the great
vessels, truncus arteriosus, and total anomalous pulmonary venous return
(TAPVR).
One other common cause of
pulmonary artery enlarge-ment is mitral disease (either stenosis or
regurgitation). In this case, increasing left atrial pressures are transmitted
to the pulmonary veins. In time, this raises pulmonary capillary wedge
pressures and eventually right heart pressures, similar to cor pulmonale from
left heart failure (see Case 3-7).
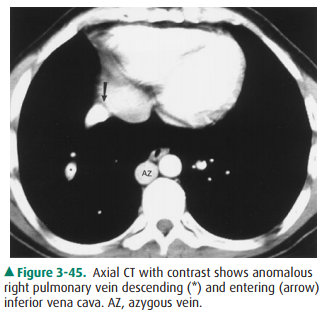
Venolobar syndrome is a form of
partial anomalous pul-monary venous return. Note the right inferior pulmonary
vein descending in a curvilinear fashion to empty into the in-ferior vena cava
(Figures 3-43 and 3-45). Right lung hypopla-sia causes the small size of the
right hemithorax and results in shift of the heart and mediastinum to the
right. Other con-genital anomalies may be present.
Pulmonary edema, as exhibited in
Case 3-15 (Figure 3-44), regardless of the cause, is another process that
causes the in-crease in the pulmonary vascularity seen on chest radiograph.
Perihilar indistinct-ness, caused by interstitial edema, may obliterate the
borders of the pulmonary vessels. Associated findings are redistribution of
blood flow to the apices, engorgement of the central veins, Kerley’s B-lines,
and pleural effusions (see Figure 3-31).
Related Topics