Chapter: Basic Radiology : Imaging of the Heart and Great Vessels
Exercise : Vascular Abnormalities
EXERCISE 3-4.
VASCULAR ABNORMALITIES
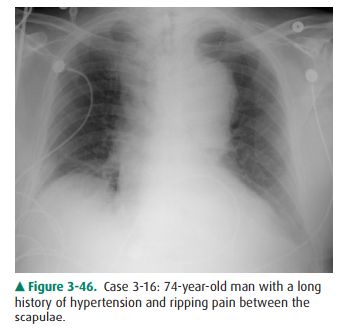
3-16. The most likely
diagnosis in Case 3-16 (Figure 3-46) is
A.
pericardial cyst.
B.
adenopathy.
C.
aortic dissection.
D.
pulmonary artery aneurysm.
E.
enlarged azygous vein.
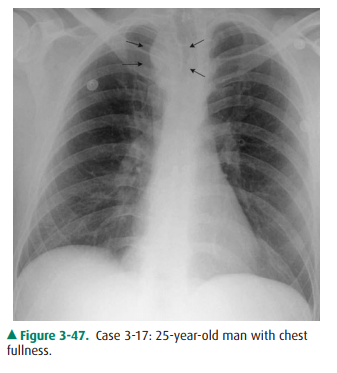
3-17. The abnormality
outlined by arrows in Case 3-17 (Figure 3-47) is
A.
substernal goiter.
B.
innominate artery aneurysm.
C.
lung cancer.
D.
right aortic arch.
E.
mediastinal adenopathy.
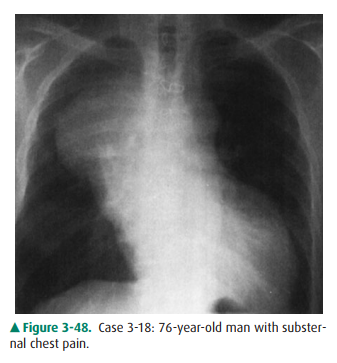
3-18. Causes for the
appearance of the chest in Case 3-18 (Figure 3-48) include all of the following
except
A.
ascending aortic aneurysm.
B.
anterior mediastinal mass.
C.
pleural mass.
D.
lung cancer.
E.
Ewing’s sarcoma of the rib.
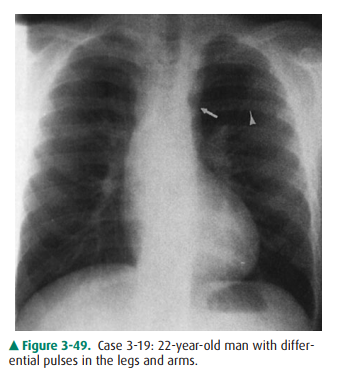
3-19. The arrow in Figure
3-49 is showing
A.
aortic ectasia.
B.
aortic constriction.
C.
pulmonary artery dilatation.
D.
adenopathy.
E.
embolic changes.
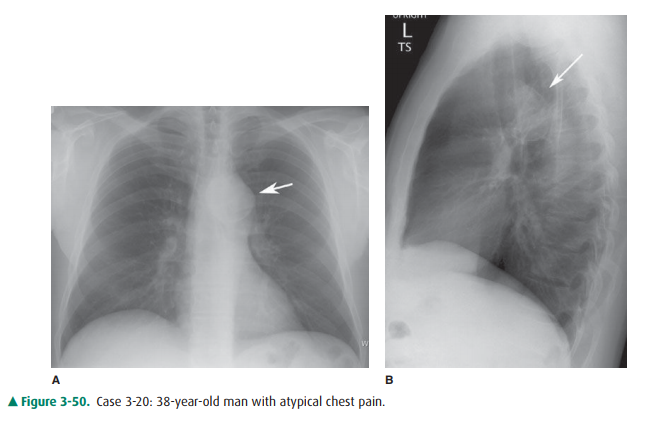
3-20. The abnormality
shown by the arrow in Figure 3-50 is most likely a(n)
A.
enlarged main pulmonary artery.
B.
descending thoracic aorta aneurysm.
C.
patent ductus arteriosus.
D.
pulmonary vein stenosis.
E.
left superior vena cava.
Radiographic Findings
3-16. In this case
(Figure 3-46), there is marked enlarge-ment of the distal ascending and
transverse thoracic aorta with shift of the trachea to the right. In
associa-tion with the clinical symptoms, the most worrisome diagnosis is
dissection of the aorta (C is the correct answer to Question 3-16).
3-17. This case (Figure
3-47) is an example of a right-sided aortic arch in an asymptomatic individual
(D is the correct answer to Question 3-17).
3-18. This case (Figure
3-48) is a radiograph of the patient in Case 3-16 (Figure 3-46) 9 years later
and shows a localized mass in the region of the ascending aorta.
The CT image (Figure 3-51)
confirmed the large as-cending aorta aneurysm (E is correct answer to Question
3-18).
3-19. This case (Figure
3-49) shows rib notching (arrow-head) and a localized constriction of the
proximal descending aorta (arrow) (B is the correct answer to Question 3-19).
These findings are diagnostic of coarctation of the aorta.
3-20. This case (Figure
3-50) is an example of a chronic pseudoaneurysm of the proximal descending
aorta (arrow) in a patient with remote major trauma (B is the correct answer to
Question 3-20).
Discussion
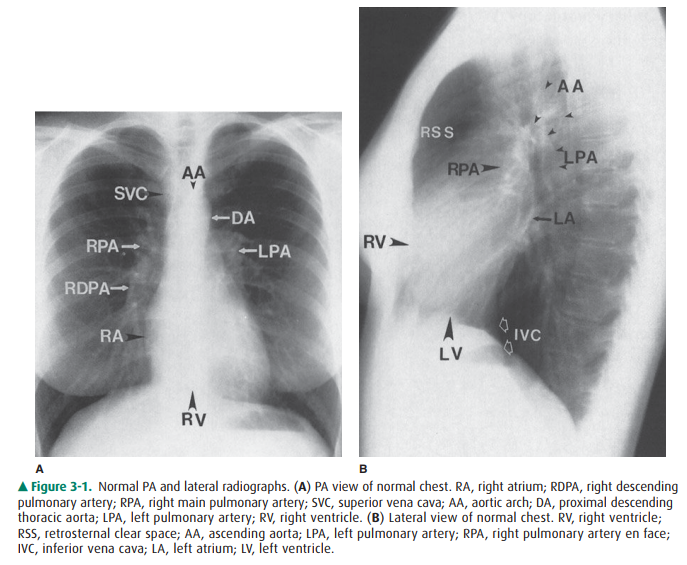
Anomalies of the major vessels
are commonly encountered on the chest radiograph. The aortic arch is an easily
recog-nized shadow. On the PA projection, the aorta originates in the middle of
the chest and then arches superiorly and slightly to the left (hence the term aortic arch), then curves, crosses the
mediastinum at an oblique angle, and continues as the descending thoracic aorta
(see Figure 3-1). The con-figuration of the aorta changes during life. In the
young person, the aortic arch is narrow and smooth and the descending thoracic
segment very straight. In the older indi-vidual with atherosclerotic disease or
aortic stenosis, the as-cending aorta becomes more prominent along the right
heart border and may have an undulating pattern in the descending thoracic
portion.
Aortic dissection as seen in Case
3-16 (Figure 3-46) can be a life-threatening diagnosis. This is often the
result of atherosclerosis and/or medial layer necrosis. In this disor-der,
blood dissects into the aortic wall through a tear of the intima. This process
may begin anywhere along the course of the thoracic aorta, but the exact
location is very important because it has therapeutic implications. Aortic
dissec-tion is most easily classified by the Stanford system. This di-vides
dissections into type A, those involving the ascending aorta, and type B, those
that begin distal to the left subcla-vian. When associated with symptoms, type
A dissections are considered surgical emergencies, whereas symptomatic type B
dissections often can be managed medically. In the acute setting, the diagnosis
is best established by CT be-cause it can rapidly define the entire scope of
the dissection as well as show the relationship to other major vessels (see
Figure 3-15). Echocardiography can also rapidly detect dis-section but provides
less anatomic detail. MR imaging is often not used in the acute setting because
of time and availability issues. The role of angiography as a diagnostic
procedure for dissection has virtually disappeared; however, intravascular
therapy including placement of stent-grafts and fenestration of the dissection
flap can be performed for treatment in many instances, including medically
inop-erable individuals.
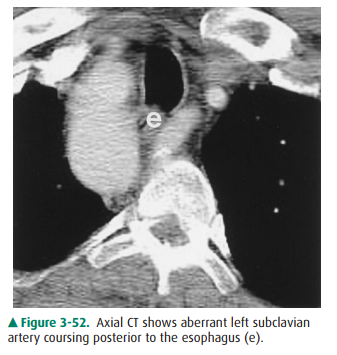
Other abnormalities of the aortic
arch are uncommon. Congenital aortic anomalies include left aortic arch with
aberrant branching, right aortic arch, and double aortic arch. The most
prominent of these aberrations is the right aortic arch, which occurs in 1 in
2500 people. It can be diagnosed on the conventional radiograph by noting an
indentation to and slight deviation of the right side of the trachea and
dis-placement of the SVC shadow, as shown in Case 3-17 (Figure 3-47, arrows).
In many individuals, the right arch is discov-ered incidentally and in these
cases, is usually associated with an aberrant left subclavian artery (Figure
3-52). The barium swallow can also demonstrate mass effect on the esophagus by
the aberrant subclavian and aorta as it crosses from right to left in the
chest. When associated with congenital anom-alies (tetralogy of Fallot, truncus
arteriosus, etc), the great vessel branching pattern is a mirror image of that
seen in a normal left aortic arch.
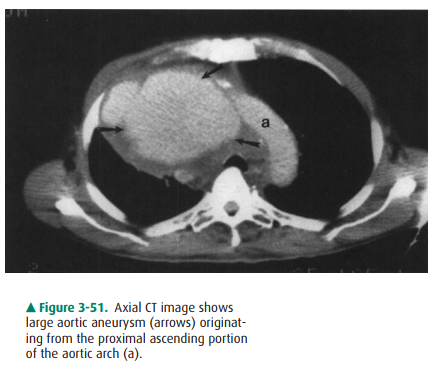
Aneurysms of the aorta, shown in
Cases 3-18 and 3-20 (Figure 3-48 and 3-50), are most often caused by
atheroscle-rosis. Trauma, infection, and connective tissue disorders such as
Marfan and Ehlers-Danlos syndrome are other causes. Aneurysms may be saccular
or fusiform in shape, and symp-toms include chest pain, hoarseness from compression
of the recurrent laryngeal nerve, postobstructive atelectasis from compression
of a bronchus, and dysphagia from esophageal compression. However, aneurysms
are most commonly dis-covered as an incidental finding on an imaging study done
for other reasons. An aneurysm of the ascending or trans-verse aortic segments
shows a focal enlargement of the aortic shadow, usually with curvilinear
calcification in its wall. A saccular aneurysm of the descending aorta may be
misdiag-nosed as a lung, mediastinal, or pleural mass, especially if it does
not contain linear calcification. In these cases, as men-tioned previously, CT
is the next best imaging modality to perform (see Figure 3-51). The lack of rib
destruction in Case 3-18 strongly argues against a chest wall sarcoma.
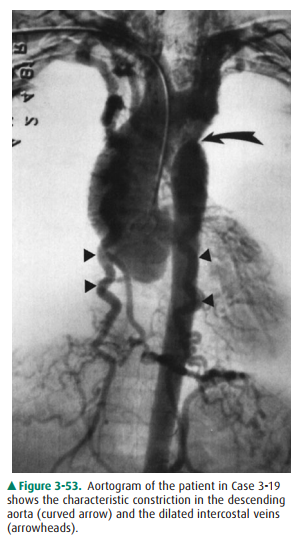
The abnormality in Case 3-19
(Figure 3-49) is coarctation of the aorta. This congenital anomaly results in
partial or complete obstruction of the aorta at the junction of the aor-tic
arch and descending aorta near the ligamentum arterio-sum (the in utero
connection between the aorta and pulmonary arteries). About one half of these
individuals also have a bicuspid aortic valve. The obstruction to flow due to
the coarctation results in elevated upper-extremity blood pressure and
decreased lower-extremity blood pressure. A systolic ejection murmur may also
be heard. Because of the partial aortic obstruction, collateral flow through
the inter-costal arteries results in the rib notching seen (Figure 3-53).
Related Topics