Chapter: Modern Medical Toxicology: Organic Poisons (Toxins): Venomous Bites and Stings
Snakebite: Clinical Features

Clinical Features
Non-Venomous Snakebite
·
A significant proportion of snakebites is said to be due to
non- venomous snakes. Since the question of envenomation does not arise in such
cases, systemic manifestations are non-existent, except those due to
psychological shock. As a result of the fear and apprehension associated with
snakes, every bite (venomous or otherwise) is attended by some degree of shock
characterised by giddiness, syncope, sweating, palpitation, tachycardia, and
hypotension. Consequent upon reassurance especially by a doctor, about the
non-venomous nature of the bite, these symptoms usually resolve rapidly.
Venomous Snakebite
1. Without Envenomation:
It is well known that even when a
highly venomous snake bites a human, serious envenomation may not occur. In
fact, it has been suggested that 20 to 50% of venomous bites are not attended
with serious toxicity.
b.
Reasons for lack of envenomation in venomous bites include the following:
·
Dry
bite: A snake does not always inject venom at thetime of biting.
·
Protective
gear: Envenomation may not occur in thecase of bites inflicted on
shod feet or heavily clothed parts.
·
Leakage of venom: Head-on bites often result in
effi-cient injection of venom, while sideswipes may cause some (or all) of the
venom to escape outside the bitesite.
·
Superficial bite: Since humans do not constitute
normalprey for most venomous snakes, they bite only to defend themselves before
making a quick get-away. In such instances, the snake often deliberately does
not bite deeply, but instead only strikes superficially, thereby conserving
precious venom for its genuine prey.
2. With Envenomation:
Colubrid bite
·
Clinical effects of colubrid
snakebite are generally localised, and comprise pain, oedema, erythema,
ecchymosis and numbness, which resolve over one to two weeks.
·
Excessive salivation with metallic
taste, and headache have also been reported.
Elapid bite
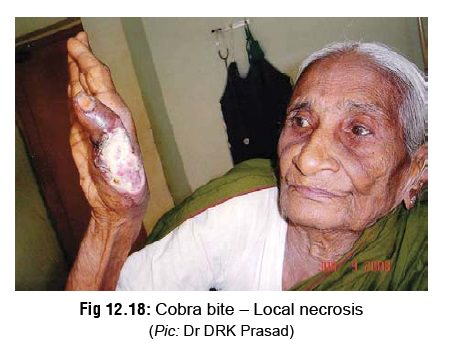
· Local Effects: In general, elapid bites are associated with minimal local manifestations (Fig 12.17). Pain and swelling are relatively less intense, and often there is only a serosanguinous ooze from the bitesite with mild pain, tenderness, and blistering. However, cobras

can
occasionally cause significant local swelling, blistering, and regional
lymphadenopathy. The lesion may emit a putrid smell, and break down with loss
of skin and subcutaneous tissue (Fig
12.18). Elapid bites sometimes cause early onset of gangrene (of the wet
type), while viperid bites progress more slowly, and the gangrene is usually of
dry type. Secondary infections, e.g. tetanus, gas gangrene, etc. are
relatively less common.
· Systemic Effects: Neurotoxicity is
the dominant clinical feature of elapid bites. Symptoms usually occur earlier
(within 15 minutes to ½ hour) in cobra bite, while they are often delayed (up
to several hours) in krait bite.
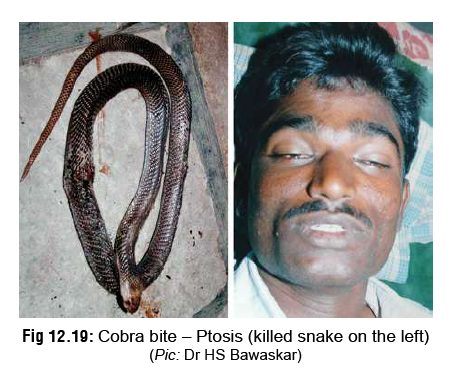
Preparalytic
Stage—
·
Vomiting
·
Ptosis (preceded by contraction of
frontalis muscle) (Fig 12.19)
·
Blurred vision, external
ophthalmoplegia
·
Paraesthesiae around the mouth
·
Hyperacusis
·
Headache, myalgia
·
Vertigo
·
Hypersalivation (due to autonomic stimulation).
Paralytic Stage—
·
The facial muscles, palate, jaws, tongue, vocal cords, neck
muscles, and muscles of deglutition
·
all become progressively flaccidly paralysed. Many patients
find it difficult to open their mouths and speak.
·
Respiratory arrest may occur due to obstruction of upper
airway by the paralysed tongue or inhaled vomitus, or due to paralysis of
inter-costal muscles and diaphragm. Paradoxical respiration, as a result of the
intercostal muscles becoming paralysed is said to be a frequent sign.
·
Although a patient appears unconscious, most are able to
follow simple commands as noted by purposeful movement of the fingers or toes.
Loss of consciousness and convulsions are terminal phenomena resulting from
hypoxaemia.
·
Roughly half of patients bitten by Naja kaouthia (monocellate cobra) do not sustain enveno-mation.
Local pain and swelling develops within 2 to 3 hours and becomes maximal in 24
to 48 hours. Blisters and skin discol-ouration may develop, and may be followed
by necrosis of subcutaneous tissue with sloughing. Neurotoxicity, if it
develops, generally begins 1 to 5 hours after envenomation, but may be delayed
as long as 19 hours. Cranial nerve palsy is followed in some patients by
generalised weakness and respiratory failure.
·
Renal complications are rare in
elapid bites.
·
Although rarely reported in literature, disorders of
platelet aggregation and coagulation-fibrinol-ysis system may occur after
envenomation by cobras. Disseminated intravascular coagulation (DIC) may occur
after bites by these snakes.
·
Coral snakes usually cause milder
manifes-tations as compared to other elapids. Even substantial envenomation is
associated with full recovery, following timely intervention.
Viperid bite
Local Effects:
– Pitless as well as pit vipers cause marked
local manifestations which develop rapidly, usually within ½ hour, but may
occasionally be delayed for several hours.
–
Swelling first appears around the bitesite,
and then spreads quickly to involve the whole limb (Fig12.20) and adjacent trunk. There is associatedpain, tenderness,
and regional lymphadenopathy. Bruising is commonly seen over the path of
super-ficial lymphatics and over regional lymph nodes.

Persistent bleeding from bitesite is
a constant feature.
– Blisters begin to appear in about 12 hours in
and around the bitesite, progressing subsequently to involve the entire limb.
They may contain either clear or bloodstained fluid. In about 10 to 15% of the
cases, extensive necrosis of skin, subcutaneous tissues, and muscles may occur.
– Raised intracompartmental pressure adds to the problem in
regions with tight fascial compartments such as anterior tibial compartment.
This is charac-terised by severe pain, tense swelling, subcutaneous
anaesthesia, and increased pain on stretching intra-compartmental muscles.
Systemic Effects:
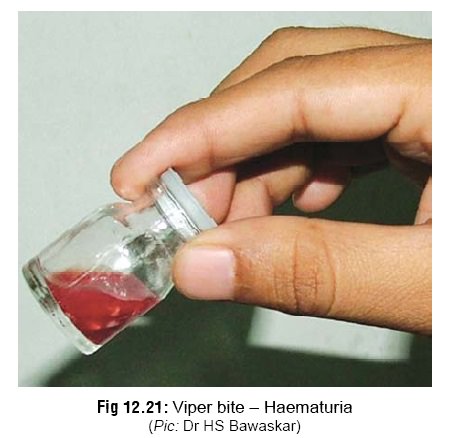
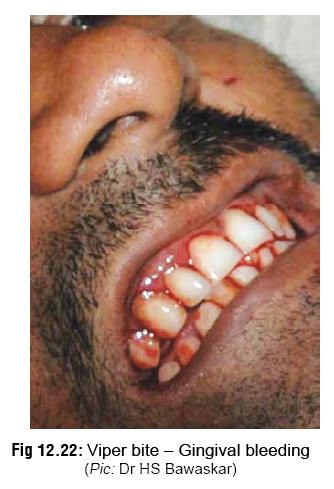
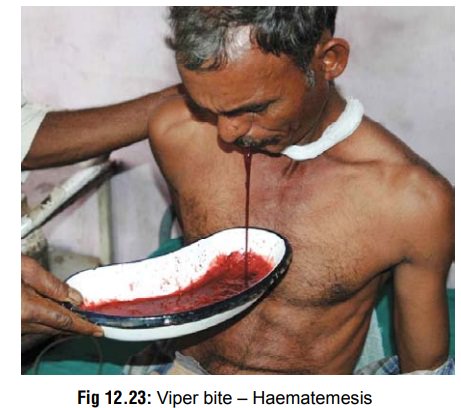
– Haemostatic abnormalities are very characteristic of viperid bites. The first evidence of this is persistent bleeding from the bitesite. Haematuria may be seen within a few hours of the bite (Fig 12.21). Later gingival bleeding occurs (Fig 12.22), followed by epistaxis, haemoptysis (relatively rare), haemate-mesis (Fig 12.23), ecchymoses, intracranial and sub -conjuctival haemorrhages, and bleeding into the floor of the mouth, tympanic membrane, gastro-intestinal tract, and genito-urinary tract. Bleeding into anterior pituitary (causing a Sheehan-like syndrome) has been reported. Subarachnoid haem-orrhage manifests as severe headache and menin-gism, while intracerebral haemorrhage may cause hemiplegia, loss of consciousness, and convulsions. Retroperitoneal and intraperitoneal haemorrhages cause abdominal distension, tenderness, and peri-tonism, with signs of haemorrhagic shock.
– Viperid envenomation is almost
synonymous with incoagulable blood, which results from defibrina-tion.
Intravascular haemolysis causing haemoglo-binuria and renal failure is a
frequent occurrence, especially in bites by Russell’s viper. Acute renal
failure is often associated with the presence of DIC which results in severe
renal tubular and cortical necrosis with widespread microvascular fibrin
deposition (microthrombi). It is suggested, however, that a direct toxic effect
produced by the venom of Russell’s viper may produce renal damage. The
hump-nosed pit viper can also cause renal failure, but the saw-scaled viper
usually does not.
–
Hypotension is an important manifestation in all viper bites and is usually
accompanied by tachy-cardia, unless the venom has affected the heart directly
or reflexly, in which case the pulse may be slow or irregular.
–
A study on saw-scaled viper bites has indicated that haemorrhagic
manifestations could more commonly be due to primary pathological fibrinolysis
(PPF) than disseminated intravascular coagulation (DIC).
The significance of this assertion
is that adminis-tration of heparin which is the treatment
of choice for DIC, may actually worsen the condition if it is due to PPF.
–
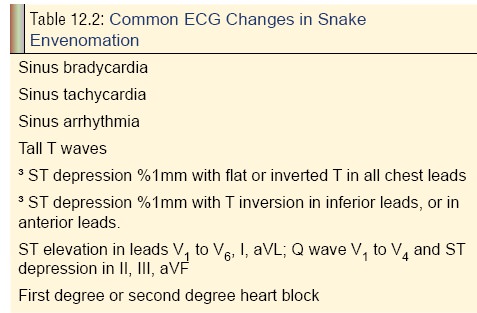
Cardiotoxicity (which may be seen in elapid bite also) produces a wide variety
of ECG changes, as listed in Table 12.2.
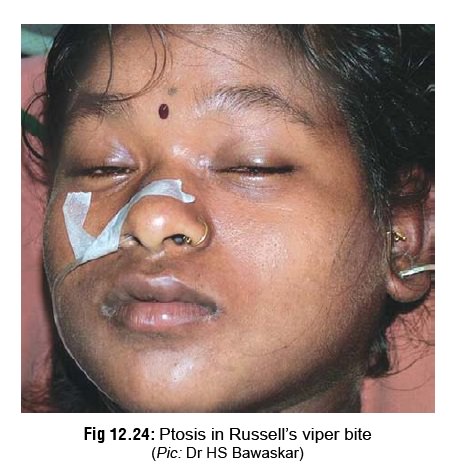
–
It is important to note that ptosis and neurological symptoms may occur in the
case of Russell’s viper bite (Fig 12.24),
and every clinician must be alert to this possibility. Generalised flaccid
paralysis can develop after envenomation. Neurotoxic effects are caused by the
presence of phospholipases A2 with presynaptic neurotoxic activity. Conversely
however, kraits and cobras do not
cause coagula-tion abnormalities.
Hydrophid bite
Local Effects: Sea snakebites are well-known to produce minimal local effects. The bite itself is often painless and the victim may not even realise he has been bitten. However teeth are often left behind in the wound.
Local swelling is negligible, and regional lymphadenitis usually does
not occur. Fang marks may appear as one, two or more small circular dots, as
though made by a pin or hypodermic needle. It is important to note that in some
cases, there may be no clear fang marks, but a vague scratch mark, and yet
serious poisoning may occur.
Systemic Effects:
–
The
dominant clinical feature is myalgia with stiff-ness and tenderness of muscles,
which become apparent in ½ hour to 2 hours. This is due to rhabdo-myolysis,
since hydrophid venom is predominantly myotoxic. Myoglobinaemia and
myoglobinuria occur, resulting in acute tubular necrosis and renal failure. A
“fixed” specific gravity of 1.010–1.013, together with a low urine volume
output, myoglo-binuria, and progressively rising blood urea are indicative of
impending acute renal failure in the setting of sea snake envenomation.
– Trismus is an early feature.
Passive stretching of muscles is painful. Later, flaccid paralysis develops,
beginning with ptosis (as in elapid bite).
–
Hyperkalaemia may be present due to release of potassium from damaged muscles.
This may be severe enough to cause cardiac arrest. Tall, peaked T waves and QRS
prolongation suggest severe hyperkalaemia.
–
Other effects may include dizziness, nausea, vomiting, headache, and
diaphoresis.
–
Neurotoxicity may include ptosis, ophthalmo-plegia, dysarthria, blurred or
double vision, mydri-asis, inability to sit unassisted, depressed muscle
stretch reflexes, and flaccid paralysis. In some cases, paralysis of
respiratory muscles causes death due to respiratory failure. Consciousness is
usually retained till the end. The fatality rate is estimated to be about 3%. Failing
vision is considered to be a terminal sign.
Related Topics