Chapter: Modern Medical Toxicology: Organic Poisons (Toxins): Venomous Bites and Stings
Brown Recluse - Venomous Arachnids
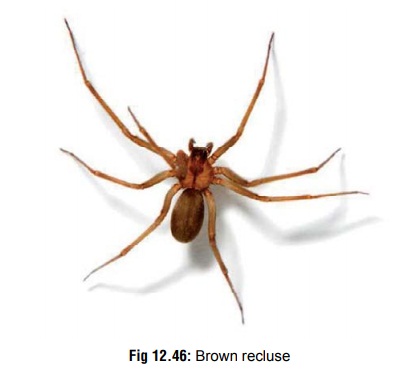
Brown Recluse
Other Common Names
·
Fiddleback, Violin, or Brown Spider.
Species
·
Loxosceles
reclusa, L. laeta, L. deserta, L. unicolor, L. arizonica, L. rufescens.
Physical Appearance
·
It is a small (6 to 20 mm long),
orange or reddish brown or grey spider, with a brown violin shaped mark on its
back (Fig 12.46). It infests dark
areas such as basements, under rocks, and amid woodpiles. The female is more
aggressive than the male and bites when provoked.

·
Loxosceles spiders can be
differentiated from most other “garden” brown spiders, of which there are many,
by its set of six eyes (three pairs), rather than eight. Their webs are
distinguished by a bluish hue.
Venom
·
The venom is cytotoxic and consists of several toxic compo- nents including hyaluronidase, ribonuclease,
deoxyribonu-clease, alkaline phosphatase, lipase, and sphingomyelinase D. The
last mentioned is the main constituent which is responsible for tissue
destruction. It reacts with sphingomy-elin in the RBC membrane causing the
release of choline and N-acylsphingosine phosphate. This causes severe
intra-vascular occlusion of micro-circulation leading to necrosis.
·
Venom toxins may act as proteases upon molecular
constitu-ents of plasma extracellular matrix (fibronectin and fibrin-ogen), and
basement membrane constituents (entactin and heparin sulfate proteoglycan). All
of these degrading activi-ties may be responsible for producing haemorrhage,
delayed wound healing, and renal failure, as well as the spreading of other
noxious toxins (e.g. dermonecrotic protein). By disrupting the subendothelial
basement membrane, blood vessel wall instability and increased permeability can
occur.
Clinical Features
1. Local
· The bite itself is usually painless, but later begins to bleed and ulcerate in 2 to 8 hours. The initial reaction often consists of erythema and pain or pruritus. A small vesicle may form at the bite area, and the lesion may take on a “bullseye” or “halo” appearance, having a central vesicle surrounded by an erythematous and ecchymotic area.
·
Ulcerated lesions if untreated, usually enlarge until about
a week when eschar formation takes place. Granulation and healing takes up to 2
months to be completed.
·
In severe cases, cutaneous necrosis
may occur and may extend to involve subcutaneous fat and muscle.
2. Systemic
·
Systemic features (“loxoscelism”) include fever, chills,
nausea, skin rash, myalgia, arthralgia, headache, vomiting, haemolysis, DIC,
shock, renal failure, jaundice, convulsions and coma.
·
Acute tubular necrosis with resulting oliguria or anuria may
develop in patients with severe haemolysis.
·
Fever is common in patients with
systemic effects and may develop more often in children. Fever may be
associated with chills and night sweats.
Diagnosis
·
Leucocytosis (20,000 to 30,000 per
cubic mm).
·
Evidence of haemolysis and DIC: Decreased levels of fibrinogen, clotting
factors, and platelets; increased levels of fi brin degradation products;
prolonged PT and PTT; spherocytosis, positive D-dimer assay, and
Coombs-positive haemolytic anaemia.
·
Abnormal renal and liver function
tests.
Treatment
1. Local
·
Wound cleansing.
·
Immobilisation of bitten extremity.
·
Tetanus prophylaxis.
·
Analgesics: Persistent pain may necessitate lumbar
sympa-thetic blocks. Application of cold compresses may help.
·
Antipruritics: Diphenhydramine 5
mg/kg/day orally, with a maximum dose of 25 to 50 mg four times a day.
Hydroxyzine may also be used: 25 to 50 mg every 6 to 8 hours; maximum dose 400
mg/day.
Antibiotics,
if wound gets infected.
2. Systemic
·
Admit patient to hospital and
monitor for evidence of haemolysis, coagulopathy and renal failure.
·
If haemoglobinuria occurs, renal failure may be prevented by
increasing IV fluids, and alkalinising urine.
·
Significant haemolysis should be
treated with transfu-sions.
Related Topics