Chapter: Modern Medical Toxicology: Organic Poisons (Toxins): Venomous Bites and Stings
Order Hymenoptera - Venomous Insects
VENOMOUS INSECTS
·
There are 3 orders of toxicological
importance in class insecta: hymenoptera, lepidoptera and
coleoptera.
ORDER HYMENOPTERA
This order comprises mainly two-winged flies and ants. The
common stinging hymenopterids include bees, wasps, yellow jackets, hornets, and
fire ants. The term “hymenoptera” refers to membranous wings that characterise
these insects.
Epidemiology
While snakebites are more common in tropical countries such
as India, anaphylactic reaction to hymenoptera stings are much more common in
temperate countries. This is despite the gross under-reporting of such stings.
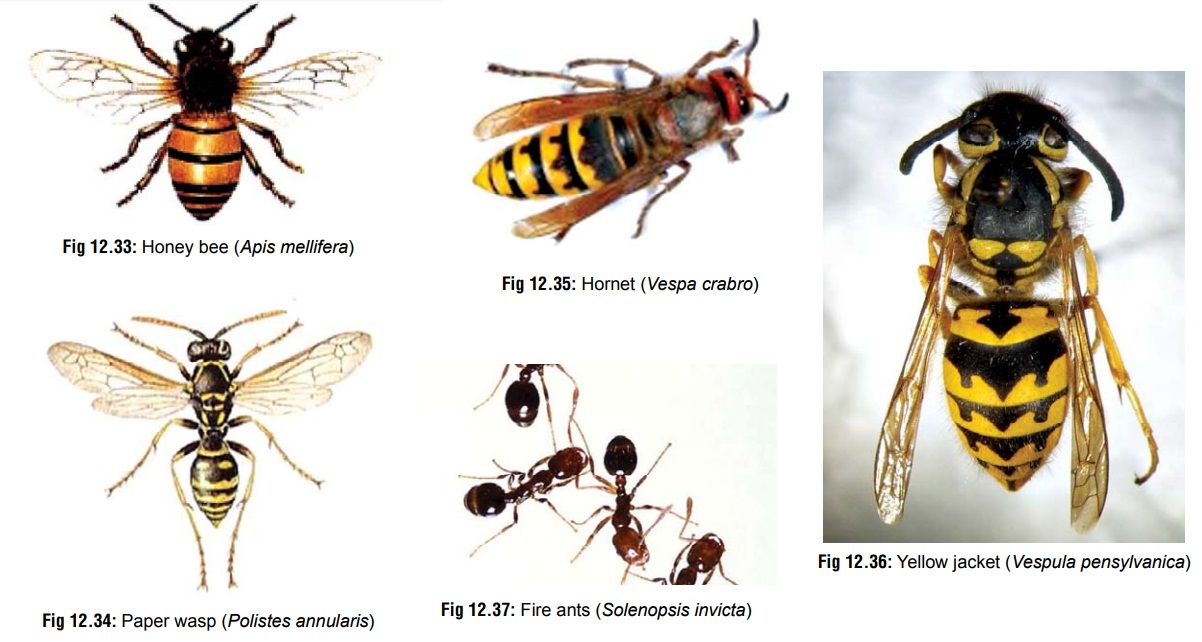
Hymenoptera stings are invariably caused by the honeybee* (Apis mellifera) (Fig12.33),
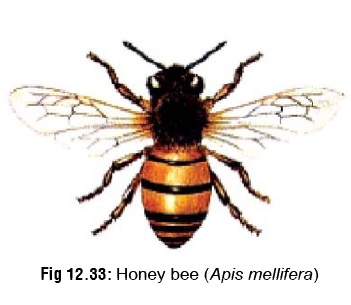
paper wasp (Polistes annularis; Ropalidia
gregaria)(Fig 12.34), European
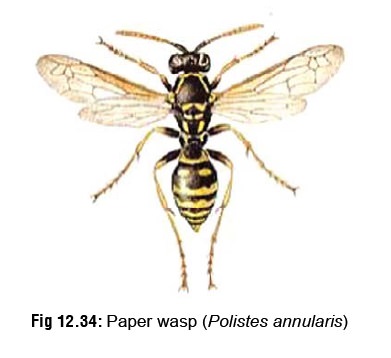
wasp (Vespula germanica), hornets (Vespa & Dolichovespula species) (Fig 12.35), and yellow jackets (Vespula pensylvanica) (Fig 12.36). A few incidents result from
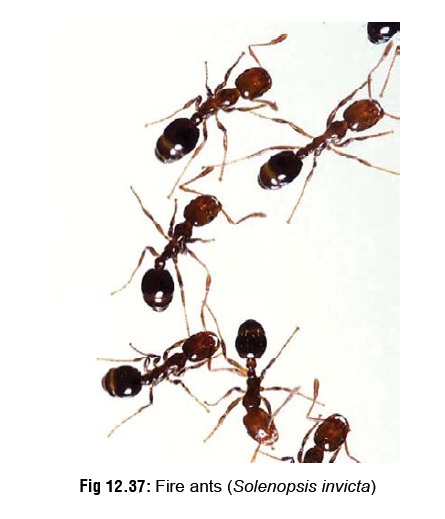
stings of fire ants (Solenopsis invicta)
(Fig 12.37), and rarely, jumper ants
(Myrmecia pilosula).


The body of a bee is generally bright yellow with black triangular markings on the abdomen. It is usually 10 to 15 mm long, and folds its wings back at rest. Queen wasps have similar markings; however, they are larger and can grow up to 20 mm. Bees are attracted to sweet food and meat and can sting multiple times. They are found in large nests, located where shelter is available (e.g. under caves, hollows of trees, and wall cavities).
Venom
Venom is usually injected through a sting which may be barbed (e.g. bee), or smooth (e.g. wasp). Bees inject approximately 50 mcg of venom which is the total capacity of the venom sac, and leave behind the stings embedded in the skin, while wasps and hornets are capable of repeated stings. Ants generally bite firmly with their jaws and then sting or spray locally irritating venom. Fire ants have well developed abdominal stingers and inflict multiple stings.
Hymenoptera venom is a mixture of biogenic amines
(histamine, 5-hydroxytryptamine and acetylcholine), enzymes (phospholipase A
and hyaluronidase), and toxic peptides (kinins in wasps; apamin, melittin, and
mast cell degranulating peptides in bees).
A complete list of the components of hymenoptera venom is
mentioned in Table 12.6.

Clinical Features
A. Local Reaction
· In individuals not allergic to the
venom, a single sting usually produces only mild effects such as local pain,
redness, irritation, itching, and swelling, which resolve in a few hours. These
reactions are not IgE-mediated, but represent a response to toxic and
inflammatory venom components such as vasoactive amines and peptides.
· Local reaction becomes dangerous
only if the site of the sting is in a vital location, e.g. mouth or tongue
(oedema leading to airway obstruction), or near the eye (cataract formation,
glaucoma, etc.). External eye stings can cause pain, swelling, lacrimation,
hyperaemia, and conjunctival chemosis. Corneal stings can cause corneal oedema,
ulceration, hyperaemia, pain, scarring, and linear keratitis.
·
Severe cutaneous infection and cellulitis have occurred
after stings from yellow jackets and wasps, which may pick up virulent bacteria
while foraging on decaying animal and vegetable matter.
B. Allergic Reactions
·
Anaphylaxis
o About
4% of the human population is hypersensitive to hymenoptera venom. Yellow
jackets and other wasps are the most serious offenders and cause twice as many
allergic reactions as honeybees. In sensitive individuals, successive stings
cause increasingly severe symptoms. Sensitisation to wasp venom is said to
occur much more rapidly than to bee venom. It is pertinent to note that there
is no association between bee or wasp sting allergy with atopy.
o Anaphylaxis
is IgE-mediated, wherein the IgE anti- bodies attach to tissue mast cells and
basophils in a previously sensitised individual. These cells are then
activated, resulting in the progression of the cascade reaction of increased
vasoactive substances such as leukotrienes, eosinophil chemotactic factor-A
(ECF-A), and histamine.
o
Clinical features develop within a few minutes of the sting,
comprising tingling sensation of scalp, flushing, dizziness, visual
disturbances, syncope, abdominal cramps, vomiting, diarrhoea, dry cough,
wheezing, and tachycardia. In severe cases, the patient develops urti-caria,
angioedema, glottic oedema, profound hypoten-sion, and coma. Hypertension has
occurred in children with multiple bee stings, and in adults with multiple wasp
stings. Apnoea, respiratory insufficiency and/or cardiopulmonary arrest have
been reported in patients who became comatose after receiving multiple stings.
Death may occur within minutes. Cardiorespiratory arrest has been reported
after multiple stings from honey bees.
o
Individuals who have had an anaphylactic reaction to a
Hymenoptera sting have a 35 to 60% chance of developing anaphylaxis from
subsequent stings by an identical insect. Atopy does not necessarily increase
the incidence of anaphylactic reactions to Hymenoptera stings, although
asthmatic patients have more severe reactions to stings than nonatopic
patients.
·
Delayed Reaction
o
A few patients develop urticaria, skin rash, pedal oedema,
and arthritis between 1 to 5 days after the sting.
o Sometimes,
a serum sickness–like syndrome occurs a week or more after the sting. This is
characterised by malaise, fever, headache, urticaria, lymphadenopathy, and
polyarthritis. Renal failure may occur rarely.
C. Toxic Reactions
·
Multiple stings (especially
involving a swarm of bees, wasps, or hornets) can cause massive envenoming
char-acterised by vasodilation, hypotension, oedema, fatigue, vomiting,
diarrhoea, headache, seizures, and coma. There have been reports of acute renal
failure.
·
Delayed toxic reactions can occur,
characterised by normal initial laboratory results, and subsequent evidence of
haemolysis, coagulopathy, thrombocytopenia, rhabdomy-olysis, liver dysfunction,
and disseminated intravascular coagulation.
·
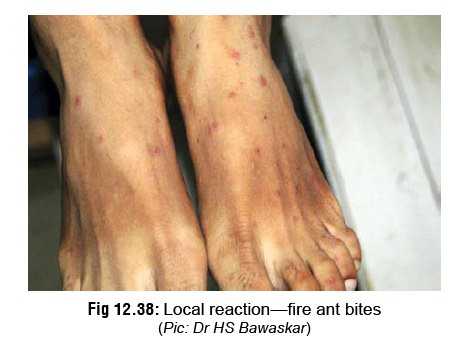
Fire ants can cause severe local reaction (Fig 12.38) and even fatal allergic
reaction (especially in young children).
High-Risk Factors
Three or more of the following risk factors are more likely
to have a major outcome or death:
·
Age 60 years or more
·
Prolonged attack time
·
High estimated number of stings
·
Medical history including
cardiovascular problems
· Early effects other than pain, such as vomiting, diarrhoea and hypotension/hypertension.
Laboratory Diagnosis
1. Diagnostic
procedures for sting allergy usually involve intradermal tests with various
dilutions of Hymenoptera venoms. Most individuals with history of
hypersensitivity to Hymenoptera stings have positive venom skin tests.
2. Intradermal skin tests are performed with
venoms diluted to concentrations in the range of 0.001 mcg to 1 mcg/ml. A
positive test is manifested by a specific wheal and flare reaction.
3. The radioallergoabsorbent test (RAST) is an “in
vitro” method that measures the quantity of venom-specific anti-bodies in the
patient’s serum, and is used as an adjunct to the venom skin test. It is
important to note that patients should not be skin tested until 2 to 4 weeks
after a Hymenoptera sting.
4.
Hymenoptera-sensitive patients should be referred to an allergist-immunologist
trained in venom immunotherapy (VIT). This consists of periodic subcutaneous
injections of the appropriate venom, starting with a low dose of about 0.01
mcg, and followed by progressively increased doses until a monthly maintenance
dose of 100 mcg (300 mcg for mixed vespid venoms) is achieved.
Treatment
Any patient sustaining multiple
stings should be observed for at least 6 hours with laboratory evaluation for
haemolysis, thrombo-cytopenia, liver and renal function abnormalities,
increased CK, and rhabdomyolysis. Patients with laboratory abnormalities, or
signs and symptoms other than local pain should be admitted.
A. Local Reaction
·
Remove embedded stinger (common in
the case of bees) by scraping with a blade or fingernail. Do not grasp the
stinger with forceps which will cause further injection of venom due to
squeezing.
·
Local infiltration with adrenaline
1:1000 (0.1–0.3 ml) near the sting site may help impede systemic absorption of
venom.
·
Local cold compress: Local application of an ice pack at the
sting site for 15 minutes every 30 minutes may decreaseintensity of swelling,
reduce pain, and help retard absorp-tion of venom.
·
Domestic meat tenderiser (papain)
diluted 1 in 5 with tap water, is reputed to produce immediate relief of pain.
·
Several other local applications have
been recommended, including topical application of 20% aluminum sulfate,
soluble aspirin, and ammonia and Epsom salt soaks. None of these treatments has
been evaluated by formal clinical trials.
·
Antihistamines: diphenhydramine (50
mg every 6 hours), chlorpheniramine (4 mg every 6 hours), or hydroxyzine (10 to
25 mg every 8 or 12 hours).
·
Local antiseptic cream.
·
Antibiotic may be administered only if there is evidence of infection.
B. Allergic Reactions
1. Anaphylaxis:
·
0.1% adrenaline (0.5 to 1 ml adult; 0.01 ml/kg child) by
subcutaneous or intramuscular injection. It
may be repeated in 20 minutes. Inhalation of adrenaline by a pressurised
inhaler is effective in relieving bronchos-pasm, but not other effects of anaphylaxis.
In life threat-ening anaphylaxis, intravenous adrenaline can be given with
extreme caution (1 ml of 1:10,000 solution diluted in 10 ml of normal saline,
given over 5–10 minutes). It can also be given as an infusion (1 mg in 250 ml
of 5 % dextrose, infused at a rate of 1 to 4 mcg/min). The dangers of
intravenous adrenaline include ventricular arrhythmias, myocardial infarction,
and death.
·
Antihistamine injection (e.g. chlorpheniramine maleate 10 mg
IV or IM, or diphenhydramine 50 mg parenter-ally, then 25 to 50 mg orally every
4 to 6 hours for 24 to 72 hours) is useful in relieving urticarial symptoms. It
can be continued for 24 to 48 hours.
·
Airway management with adequate
ventilation and oxygenation: Oxygen—5 to 10 L/min via high flow mask.
·
Bronchodilators such as salbutamol
to relieve dyspnoea and wheezing.
·
Corticosteroids:
–
Methylprednisolone—1 to 2 mg/kg IV every 6 to 8 hours.
–
Prednisone—Adults: 40 to 60 mg/day. Children: 1 to 2 mg/kg/day (divided
twice daily).
–
Large doses of hydrocortisone may be required to help the resolution of massive
oedema.
·
Correction of hypotension and shock:
Dopamine and IV fluids.
·
Continuous cardiac monitoring.
·
Since rebound anaphylaxis can occur
in some patients (up to 10 hours after a sting), observe every patient for 10
to 12 hours before discharging.
2. Delayed reaction:
·
Antihistamines
·
Analgesics
·
Haemodialysis for renal failure.
Preventive Measures Against Hymenoptera Stings
·
Individuals who have recovered from
anaphylaxis following an insect sting must be trained to self-admin-ister
adrenaline. They should carry a pre-loaded syringe of adrenaline when moving
about in hymenoptera-infested areas.
·
Patients known to be hypersensitive
should wear an identifying tag as they may be discovered unconscious after a
sting.
·
Hymenoptera nests in areas around the living or working
quarters of a sensitised patient should be destroyed.
·
When moving outdoors, tight, light-coloured, long-sleeved
clothing should be worn.
·
Clothing with bright floral patterns should be avoided when
moving about in gardens, or while working with plants.
·
Attractive scents, perfumes, soaps,
and shampoos must not be used when moving in high-risk areas.
·
Materials or plants that attract
hymenoptera (e.g. cloves, dandelions, open sweet drinks, etc) must be reduced.
·
Drinking juices or honey directly out
of cans and bottles is a common cause of stings in the mouth and pharynx, and
therefore should be avoided.
·
If individuals with venom
sensitivity are taking beta-blockers or non-steroidal analgesic drugs, these
should be withdrawn whenever possible, as both potentiate anaphylaxis.
·
Angiotensin-converting enzyme
inhibitors and calcium channel antagonists may aggravate cardiovascular
response to anaphylaxis, and should be substituted with other drugs if
possible.
·
Adults with a history of significant
allergic reactions to hymenoptera stings may benefit from desensitisation
(immunotherapy).
Related Topics