Chapter: Modern Medical Toxicology: Neurotoxic Poisons: Anaesthetics and Muscle Relaxants
Propofol - Intravenous Anaesthetics
Propofol
Propofol (2,6-diisopropylphenol) is a synthetic intravenous
anaesthetic which is an oil at room temperature and is supplied as a 1% emulsion
(in 10% soyabean oil, 2.25% glycerol, and 1.2% purified egg phosphatide).
Uses
■■ Propofol is useful
in the induction and maintenance of general anaesthesia as part of inpatient or
outpatient surgery in adults and children over 3 years of age.
■■ The exact mechanism
of action is unclear but is probably related to its ability to enhance
GABA-mediated synaptic inhibition.
Adverse and Toxic Effects
·
Propofol is known to cause hypotension, bradycardia, and
even cardiac arrest.
·
In children, it may induce choreiform movements, rigidity,
and ataxia if the usual dose is exceeded.
·
Some paediatric cases have demonstrated high morbidity
associated with lipaemic serum and elevated levels of very-low-density
lipoproteins and triglycerides. Whether this has any relationship to the lipid
carrier of propofol is not clear.
·
Several paediatric case reports of “propofol infusion
syndrome” following prolonged propofol use for inten-sive care sedation have
been described. The syndrome, which may be fatal, is characterised by metabolic
acidosis, bradyarrhythmias, rhabdomyolysis, hyperka-laemia, hyperlipaemia, acute
renal failure, massive keto-nuria, elevated liver enzymes, fatty liver and
myocardial failure. Biochemical findings are consistent with impaired ![]() fatty-acid oxidation; the resultant
lack of substrates and the build-up of intermediaries in the metabolism of
long-chain, medium-chain, and short-chain fatty acids could theoretically
account for the clinical features present. Although children are said to be
more likely to develop this condition, adults have also been affected.
Fatalities have occurred in both groups.
fatty-acid oxidation; the resultant
lack of substrates and the build-up of intermediaries in the metabolism of
long-chain, medium-chain, and short-chain fatty acids could theoretically
account for the clinical features present. Although children are said to be
more likely to develop this condition, adults have also been affected.
Fatalities have occurred in both groups.
·
Fever has been associated with prolonged propofol infu-sion
in children.
·
Anaphylactic reactions have occurred during propofol
administration.
·
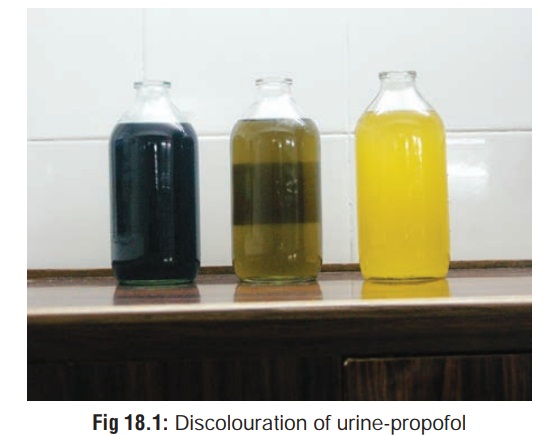
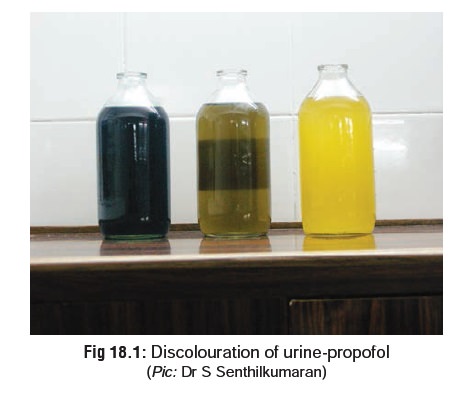
Discoloured urine (olive green, rusty brown, tea-coloured)
has been reported in several paediatric exposures to prolonged propofol
infusions used for intensive care sedation (Fig 18.1).
·
Complex external ophthalmoplegia has been reported in
patients recovering from propofol anaesthesia.
·
It appears that propofol has both anti-convulsant and
pro-convulsant activity. There have been several reports of seizure activity
following the use of propofol. Seizures or excitatory effects have been
reported during induction, immediately after anaesthesia and delayed (sometimes
for up to several days after surgery) following the use of propofol. Several
possible mechanisms have been suggested:
––
Propofol has a primary action at or close to the GABA receptor with a much
lower level of glycine antagonism responsible for the excitatory effects
–– Antidopaminergic action
––
Imbalance between cortical and subcortical effects with propofol is involved
with the symptoms observed.
Propofol is susceptible to contamination with micro-organisms (S.aureus, E.coli, P.aeruginosa, C.albicans, etc.), and cases have been recorded where bacteraemia has resulted from its use in patients. It is recommended that propofol ampoules should be wiped with alcohol before use, and strict aseptic techniques should be followed when preparing infusions.
Treatment
·
Monitor arterial blood gases in all patients following a
significant exposure.
·
Monitor ABGs routinely in children receiving propofol
infusions for a prolonged period or in patients as indi-cated.
·
Obtain baseline electrolyte levels and monitor fluid status.
·
Monitor ECG and blood pressure in patients following
overdose or prolonged exposure.
·
Establish respiration and create an artificial airway if
necessary. Check adequacy of tidal volume.
·
Aggressively treat and evaluate coma. Intubate and ventilate
as needed.
·
Physostigmine may help in central anticholinergic syndrome
(especially if it is asociated with hypotension and arrhythmias), but must be
used with caution.
·
Atropine is useful in bradycardia. For ventricular
arrhythmias, obtain an ECG, institute continuous cardiac monitoring and
administer oxygen. Evaluate for hypoxia, acidosis, and electrolyte disorders
(particularly hypokalaemia, hypocalcaemia, and hypomagnesaemia). Lignocaine and
amiodarone are generally first line agents for stable monomorphic ventricular
tachycardia, particularly in patients with underlying impaired cardiac
function. Sotalol is an alternative for stable monomor-phic ventricular
tachycardia. Unstable rhythms require cardioversion.
·
If there is evidence of metabolic acidosis, with a pH of
less than 7.1 administer sodium bicarbonate at 1 to 2 mEq/kg every 1 to 2
hours. Repeat ABGs to evaluate response.
·
For rhabdomyolysis, early aggressive fluid replacement is
the mainstay of therapy and may help prevent renal insufficiency. Diuretics
such as mannitol or furosemide may be needed to maintain urine output. Urinary
alka-linisation is NOT routinely recommended.
Related Topics