Chapter: Modern Medical Toxicology: Neurotoxic Poisons: Anaesthetics and Muscle Relaxants
Cocaine and Other Local Anaesthetics
LOCAL ANAESTHETICS
Cocaine
· Cocaine is present in the leaves of the coca plant (Erythroxyloncoca) and is an ester of benzoic acid and methylecgonine.Local anaesthetic effect is due to blockade of nerve impulses. It also has local vasoconstrictive effect secondary to inhibition of norepinephrine re-uptake. Cocaine hydrochloride is used as a 1%, 4%, or 10% solution for topical application. Its use is greatly restricted because of its toxicity and abuse potential. Cocaine is mainly used as a local anaesthetic for the upper respiratory tract.
Other Local Anaesthetics
· Procaine, introduced in 1905, was the first synthetic local anaesthetic and is an amino ester. The other amino esters include amylocaine, benzocaine, butacaine, chloroprocaine, cyclomethycaine, hexylacaine, isobucaine, meprylcaine, oxybuprocaine, piperocaine, proparacaine (proxymetacaine), propoxycaine, tetracaine (amethocaine), and of course cocaine.
· A second group of local anaesthetics comprise the amino amides—articaine, bupivacaine, butanilicaine, carticaine, dibu-caine (cinchocaine), etidocaine, lignocaine (lidocaine), mepiva-caine, oxethazaine, prilocaine (propitocaine), and ropivacaine.
· A third group of miscellaneous agents include diperidon, dyclonine, and pramoxine.
· The most commonly used local anaesthetics are lignocaine and bupivacaine. A mixture of lignocaine (500 to 1000 mg/L), adrenaline (0.25 to 1 mg/L) and sodium bicarbonate (12.5 mmol/L) in 0.9% saline is usually infused into the surgical site for local anaesthesia, and to minimise blood loss during tumes-cent liposuction. Doses of lignocaine during this procedure can reach 55 mg/kg. Death can result from severe bradycardia and hypotension during such a procedure.
Mode of Action
· Local anaesthetics reversibly block the generation and conduction of nerve impulses. The blockade progresses as follows: peripheral vasodilation, rise in skin temperature, loss of pain sensation, loss of temperature sensation, loss of proprioception, loss of touch and pressure sensation, and finally motor paralysis.
· Local anaesthetics produce a conduction block at the cell membrane of the involved nerve. All nerves (sensory, motor, and autonomic) are affected, but small diameter pain/temperature (AS fibres) and autonomic ones (B and C fibres) are most susceptible. This conduction block is eventually reversible and is produced by a transient increasein sodium permeability, which would normally produce the action potential and permit its propagation.
· Anaesthetics prevent the increase of sodium pump perme- ability which occurs during normal impulse transmission. They also interfere with permeability of potassium in the resting nerve. The permeability of both sodium and potas- sium are calcium dependant and it is believed that local anaesthetics compete with calcium for membrane binding sites.
· Local anaesthetics also have intrinsic vasodilator activity.
Toxicokinetics
· Local anaesthetics are absorbed from mucosal surfaces as well as from parenteral sites. They are rapidly absorbed from the GI tract with peak plasma levels occurring within 30 to 60 minutes.
· Peak blood concentrations occur within 10 to 15 minutes of intramuscular lignocaine administration. Peak blood levels occur within 30 to 45 minutes of caudal, epidural, periph- eral nerve block, or infiltration anaesthesia. Absorption is retarded by co-administration of a vasoconstrictor (e.g. adrenaline). There is significant first-pass hepatic metabo-lism of amide-type agents (65% for lignocaine).![]()
· Protein binding: bupivacaine—82 to 96%; etido-caine—96%; lignocaine—51 to 80%; mepivacaine—60 to 85%; prilocaine—55%; tetracaine—76%.
· Volume of distribution: bupivacaine—0.4 to 1 L/kg; etido-caine—1.9 L/kg; lignocaine—1.1 L/kg; mepivacaine—1.2 L/kg; procaine—0.3 to 0.8 L/kg.
· Agents of the ester type are rapidly metabolized mainly in the plasma by pseudocholinesterases yielding para— aminobenzoic acid derivatives. They are also metabolised to a small degree by liver esterases. Agents with an amide linkage are metabolised by hepatic microsomal enzymes.
· Metabolites of both types of compounds are excreted in the urine. Only small amounts of parent drug are excreted unchanged.
· Elimination half—life: articaine—20 to 120 minutes;bupivacaine—1.3 to 5.5 hours; etidocaine—1 to 2.7 hours; lignocaine—1.5 to 2 hours; mepivacaine—1.9 hours; prilo-caine—1.5 hours; procaine—7 to 8 minutes.
Adverse Effects
· Toxicity is due to an exaggerated pharmacological activity, primarily involving the cardiovascular and central nervous systems. High drug levels result in depressed membrane func-tion of all excitable tissues eventually resulting in membrane instability.
· Dyclonine has a different chemical structure than “caine” type anaesthetics. Hypotension is due to reduced cardiac output and peripheral vasodilation. At high doses, respiratory stimula-tion, followed by respiratory depression occurs. Unlike other local anaesthetics, dyclonine has anticonvulsant activity.
Clinical (Toxic) Features
· Allergic Reactions: Generally rare and usually associated with ester compounds.
o Idiosyncrasy—Vasovagal attack or hysterical reactions. Anxiety, panic attacks, hallucinations, and psychotic reactions have occurred.
o Local Effects—Accidental subarachnoid injection of chloroprocaine may cause adhesive arachnoiditis or cauda equina syndrome. Intravenous use is associated with venous thrombosis.
o Systemic Effects – Usually result from inadvertent intravascular injection of local anaesthetics. The following manifestations occur: perioral numbness, tingling, auditory and visual disturbances, twitching, convulsions, cardiac arrhythmias, coma, and death. Sometimes there is flaccidity, apnoea, coma, and circulatory collapse. Urticaria and angioedema may accompany systemic allergic reactions. Other derma-tological effects include contact dermatitis, generalised burning and numbness and pruritus. Vasodilation, with pink skin, has been reported.
· Systemic Toxicity: Toxicity may occur after ingestion, topical use, or parenteral administration. It may result from an excessive dose, mistaken drug identity, enhanced ![]() drug absorption, inadvertent intravascular injection, altered protein binding, slowed redistribution and/or elimination.
drug absorption, inadvertent intravascular injection, altered protein binding, slowed redistribution and/or elimination.
o Cardiac arrhythmias, myocardial depression, and cardiovascular collapse due to profound vasodila-tion. Toxic doses of local anaesthetics depress cardiac conduction and contractility, causing arrhythmias (sinus bradycardia, AV junctional or ventricular bradycardia, second or third degree heart block, asystole; rarely ventricular tachycardia or fibrillation due to re-entrant mechanisms). A transient period of tachycardia and hypertension may precede bradycardia, hypotension, and asystole. Heart block occurs more readily in patients with concomitant therapy with calcium channel blockers and beta blockers. ECG manifestations include sinus bradycardia, atrioventricular block, increased PR and QRS intervals and asystole.
o CNS effects invariably precede significant cardiovas-cular toxicity, except following massive IV injection. Subjective effects after therapeutic doses or in mild toxicity include drowsiness, impending doom, head-ache, dizziness, paraesthesias, euphoria, numbness of the mouth, light-headedness, tinnitus, anxiety, confu-sion, tremors, agitation, disorientation, hallucinations and lethargy. While there is often a progression of symptoms after IM, SC, or continuous IV infusion, seizures and coma may occur suddenly after rapid IV administration. Most of the local anaesthetics are anti-convulsants at low doses and convulsants at high doses. Seizures can occur regardless of route of administration, though they are more common with IV use.
o Nausea and vomiting.
· Miscellaneous Effects:
o Lignocaine IV may cause sudden apnoea and asystole.
o Bupivacaine is known to cause QRS prolongation even with proper administration of therapeutic dose. It is more cardiotoxic than lignocaine.
o Prilocaine can cause methaemoglobinaemia since it is an aniline derivative.
o Structurally different from the benzoate esters or the amides, pramoxine is reported to have relatively “low systemic toxicity”. It also does not cause sensitisation as frequently as benzocaine, yet is an equally effective anaesthetic.
o Exposure to prilocaine, benzocaine, lignocaine, tetracaine, or cetacaine may result in methaemoglo-binaemia. The aetiology is metabolism to o-toluidine and 4-hydroxy-2- methylaniline, both known methae-moglobin inducers.
o Ring keratitis, corneal oedema, Descemet’s membrane folds, and a subtotal corneal epithelial defect have been described after abuse of topical ocular anaesthetics.
o Local anaesthetics readily cross the placenta. Foetal or neonatal poisoning may occur as a result of spinal or regional nerve blocks, systemic maternal poisoning, or inadvertent intracranial injection of local anaesthetics into the foetus during labour and delivery. Bupivacaine is contraindicated in obstetrical paracervical block anaesthesia. Use of bupivacaine in obstetrical paracer-vical block has resulted in foetal bradycardia and death.
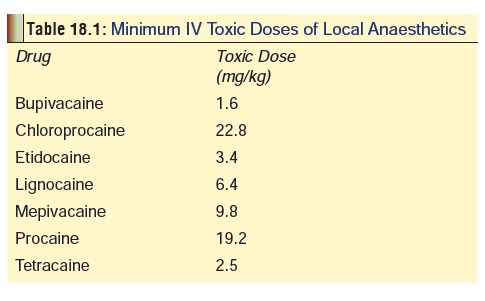
Usual Fatal Dose
The minimum IV toxic doses of some local anaesthetics are listed in Table 18.1. The single dose limit for lignocaine is 2 mg/kg for IV doses and 3 to 4.5 mg/kg for infiltration, nerve block, or regional anaesthesia. When administered with adrenaline for local anaesthesia, the total dose should not exceed 7 mg/kg. Fatalities can occur upon intravascular injection of therapeutic (infiltration/nerve block) doses.
Diagnosis
· Therapeutic levels of lignocaine vary between 1 to 5 mcg/ ml. Serious poisoning may occur at levels above 5 mcg/ml for lignocaine, mepivacaine, or procaine. For bupivacaine, therapeutic plasma concentrations are less than 3 mcg/ml. Bupivacaine is more toxic than lignocaine when given intravenously. For etidocaine, peak plasma concentrations following therapeutic doses range from 0.5 to 1.5 mcg/ml.
· Serum protein (alphal-acid glycoprotein) concentrations must be considered when interpreting lignocaine levels, since assays generally measure total drug concentration. Free drug levels may be relatively higher in patients with low protein concentrations.
Treatment
· Maintain airway; ventilate with 100% oxygen.
· Treat acidosis (presence of acidosis increases toxicity). Consider sodium bicarbonate in patients with severe meta-bolic acidosis. A reasonable starting dose is 1 to 2 mEq/ kg. Monitor serum electrolytes and arterial blood gases. Respiratory acidosis should be corrected by assisted ventila-tion.
· Treat convulsions with thiopentone IV (50 to 100 mg), diazepam (10 mg), or midazolam (2 mg). Attempt initial control with a benzodiazepine. If seizures persist or recur administer barbiturates. Phenytoin may worsen cardiac arrhythmias and should be avoided.
· Treat hypotension with IV fluids, pressors (e.g. dopamine), Trendelenberg position.
· Treat bradycardia with atropine, tachycardia or ventricular fibrillation with electrical cardioversion, or bretylium (5 mg/kg IV).
· Acute lignocaine toxicity can usually be managed with supportive measures. Massive overdose may necessitate atrioventricular cardiac pacing, or extracorporeal pump assistance.
· Bupivacaine-induced cardiac arrest may respond to cardio-pulmonary bypass.
· Methaemoglobinaemia resulting from lignocaine and prilo-caine can be treated with methylene blue (1 to 2 mg/kg/dose or 0.1 to 0.2 ml/kg/dose IV over 5 minutes as needed every 4 hours).
· Haemodialysis, exchange transfusion, AV haemofiltration and forced diuresis have not been shown to substantially increase clearance. Urinary acidification is not recom-mended. Although acidification of the urine will enhance the excretion of local anaesthetics, the contribution to overall elimination is small, and the risk of such therapy outweighs the benefit.
Forensic Issues (Anaesthetics)
· In contrast to earlier years, anaesthesia is asociated with low mortality today and is estimated to be just 1 in 10,000 with proper care in administration.
· Low blood volume, underventilation, aspiration and vomiting, and collapse following intravenous block are the main factors in the few deaths reported.
· Increased susceptibility to mortality is associated with heart disease, advanced age, and high-risk surgery (cardiovas- cular, thoracic, abdominal, or neurologic).
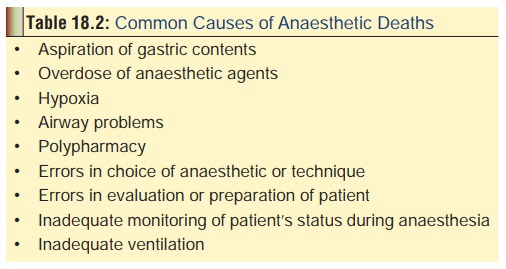
· Table 18.2 mentions important causes of death during anaesthesia.
· Pregnancy is not associated with significant enhancement of mortality. However some studies suggests an increased risk for congenital anomalies (hydrocephalus and eye defects) in babies born to mothers who had been administred general anaesthetics in the first trimester.
· There is evidence to suggest that operating room workers may suffer from the results of occupational exposure to general (inhalational) anaesthetics if precautions are not taken – proper connection of scavenging equipment, turning the gas off when breathing system is discon- nected from patient, and use of properly fitting masks on patients.
· Anaesthetic agents are not uncommonly employed for suicide. Homicides are rare.
· Anaesthetic drug abuse is a significant problem among
· anaesthesia personnel in the Western countries, while similar data are not available in the Indian context.
· Common agents abused include alcohol, narcotic drugs, barbiturates, tranquillisers, and nitrous oxide. Halothane and ketamine are also being increasingly abused. Even topical ocular anaesthetics may be abused by hospital personnel which may lead to keratitis, corneal damage, and visual loss.
· Ketamine, as well as fentanyl and its derivatives are known for their abuse potential even among the general population (discussed in earlier sections). Ketamine, like phencyclidine, has become a popular drug of abuse in several Western countries. Users apparently desire the hallucinogenic side effects. Chronic use can result in tolerance requiring increasing dosages of ketamine to produce the same effects. The following long-term adverse effects have been associated with ketamine abuse: flashbacks, hallucinations, attentional dysfunction, memory impairment, tolerance, and a high degree of dependence. Signs and symptoms of ketamine withdrawal may include chills, autonomic arousal, lacrimation, restlessness, visual, olfactory, and tactile hallucinations, nightmares and psycho- logical cravings.
· Nitrous oxide is used as a propellant gas in food aerosols (i.e. foaming agent for whipped cream). “Whippet” is a slang term for a cylinder or cartridge designed to charge whipped cream dispensers. The term “nanging” has also been used to describe the recreational use of this agent via cartridges of nitrous oxide. Widespread abuse of this agent has been reported in the United States. These cartridges may be commercially available in supermarkets (Australia), adult bookstores, bar supply shops, and by mail order. Individuals abusing this agent may also purchase it in a can of cooking oil preparation or whipping cream, where it is used as a propellant. The can is inverted and sprayed for a short time until no further oil or whipping cream comes out and only the gas is being emitted from the nozzle. The gas is sprayed into a plastic bag and breathed or sniffed directly. Fatalities are usually due to suffocation and a plastic bag may be found near the victim’s head.
· Propofol is increasingly being used as an intravenous drug of abuse. In one report, several young males employed at health care centers were arrested for erratic driving behaviour and were found to be injecting themselves with propofol. The famous pop star Michael Jackson (Fig 18.2) is alleged to have died due to an overdose of propofol that was being administered to him by his personal physician to help him sleep, since he suffered from severe insomnia.

· Procaine may produce a stimulant effect, similar to cocaine, when inhaled and is sometimes called “synthetic cocaine”. Powdered procaine is commonly used to “cut” cocaine and has been sold as cocaine when mixed with mannitol or lactose.
Related Topics