Chapter: Medicine and surgery: Hepatic, biliary and pancreatic systems
Portal hypertension - Complications of chronic liver disease
Complications of chronic liver disease
Portal hypertension
Definition
Raised portal venous pressure is usually caused by increased resistance to portal venous blood flow and is a common sequel of cirrhosis. When the portal venous pressure is consistently above 25 cm H2O, serious complications may develop.
Aetiology
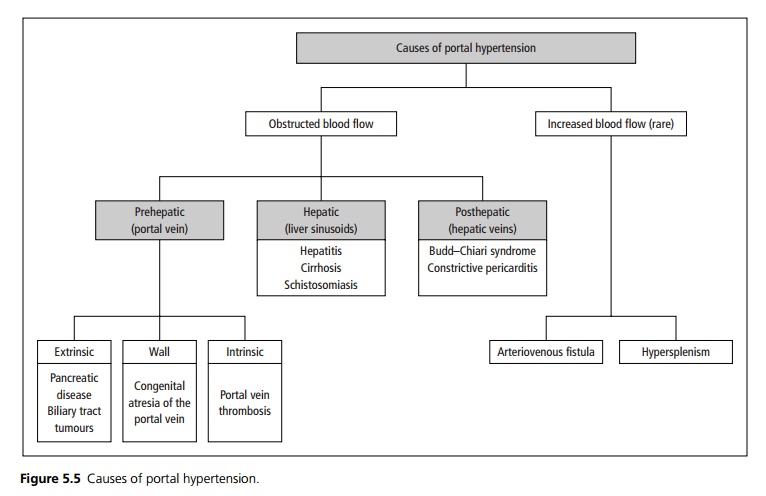
By far the most common cause in the United Kingdom is cirrhosis of the liver. Causes may be divided into those due to obstruction of blood flow, and rare cases due to increased blood flow (see Fig. 5.5).
Pathophysiology
Venous blood from the gastrointestinal tract, spleen and pancreas (and a small amount from the skin via the paraumbilical veins) enters the liver via the portal vein. As the portal vein becomes congested, the pressure within it rises and the veins that drain into the portal vein become engorged. If the portal pressure continues to rise the flow in these vessels reverses and blood bypasses the liver through the portosystemic anastamoses (paraumbilical, oesophageal, rectal). This portosystemic shunting eventually results in encephalopathy.
Clinical features
The presenting symptoms and signs may be those of the underlying disease, (most commonly cirrhosis), of reduced liver function or features of portal hypertension. Portal hypertension causes oesophageal varices, splenomegaly, distended paraumbilical veins (caput medusa), ascites and encephalopathy.
Complications
Oesophageal varices can cause acute, massive gastroin-testinal bleeding in approximately 40% of patients with cirrhosis. Anorectal varices are common, but rarely cause
Investigations
These are aimed at discovering the cause of the portal hypertension and assessing the degree of portal hypertension, when considering surgical intervention. The severity of liver disease may be graded A–C by means of a modified Child–Pugh grading system. Ultrasound of the liver and spleen is performed to assess size and appearance. Additional Doppler studies can assess the direction and flow of blood within the portal and hepatic veins. Liver biopsy may be required. The hepatic wedge pressure may be directly measured.
Management
· Portal hypertension is significantly improved by abstinence from alcohol in cases of alcoholinduced disease.
· Primary prophylaxis against variceal haemorrhage:
1. β-blockers, in particular propranolol, cause splanchnic vasoconstriction and reduce cardiac output. This reduces the portal pressure gradient, the azygos blood flow and variceal pressure, which reduces the likelihood of variceal bleeding.
2. Endoscopic variceal band ligation may be performed in patients with significant varices who are unable to tolerate β-blockers.
3. If both β-blockers and endoscopic banding are contraindicated isosorbide mononitrate has been shown to be effective.
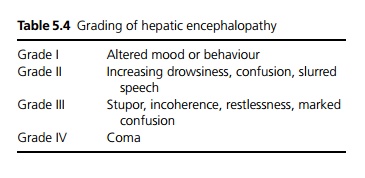
Specific complications requiring intervention include ascites, bleeding varices and encephalopathy (see Table 5.4).
Portosystemic shunting is used in patients with reasonably good liver function and who are not being considered for a liver transplant. There are various techniques, for example connecting the:
1. 1 Portal vein to inferior vena cava.
2. 2 Splenic vein to left renal vein (Warren shunt): useful for portal vein obstruction and maintains liverblood flow, so that there is a lower risk of encephalopathy afterwards.
3. 3 Insertion of a transjugular intrahepatic portosystemic shunt (TIPSS) can be performed without general anaesthesia and laparotomy. A transjugular approach is used to pass a guidewire through the hepatic vein piercing the wall to the intrahepatic branches of the portal vein, a stent is then passed over the guidewire. The risk of encephalopathy is the same as for other shunts, but operative morbidity and mortality is improved.
Liver transplantation offers the only hope of cure.
Related Topics