Chapter: Medicine and surgery: Hepatic, biliary and pancreatic systems
Liver function testing - Investigations and procedures
Investigations and procedures
Liver function testing
Liver function testing includes blood tests to look for evidence of hepatocyte necrosis, as well as assessing the actual functions of the liver, i.e. its synthesis of proteins including albumin and clotting factors and bile metabolism and excretion. In most laboratories, if liver function tests (LFTs) are requested, this means measurement of the serum levels of bilirubin, aminotransferases, alkaline phosphatase (ALP) and total protein. γ -glutamyl transpeptidase (γ -GT) may be included amongst the standard tests, but often needs to be requested separately. For assessing the synthetic function of the liver, two other blood tests are needed, the prothrombin time and serum albumin.
Hepatocyte necrosis/damage
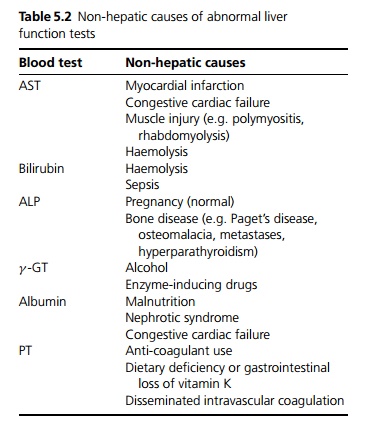
Aminotransferases: Two are measured, aspartate aminotransferase (AST) and alanine aminotransferase (ALT). These are raised by most causes of liver disease, but paradoxically, in severe necrosis or in late cirrhosis levels may fall to normal indicating a lack of viable hepatocytes. ALT is more specific than AST, the latter being found in many other organs (see Table 5.2).
Obstruction
Bilirubin: Raised bilirubin levels indicate abnormalities in its synthesis, metabolism or excretion. It often rises in causes of obstructive (cholestatic) jaundice, but it is not specific for obstruction or even for liver disease (see Table 5.2 and page 185).
ALP: This enzyme is found in the liver, where it is produced by the cells lining the small bile ducts. It is also found in bone, placenta and intestine. If the liver disease is primarily due to obstruction of the intrahepatic or extrahepatic bile ducts (cholestatic), the ALP rises first and proportionally more than the aminotransferases.
If the ALP is raised due to liver disease, γ -GT measurement is also raised as it shares a similar pathway of excretion. If γ -GT levels are normal with a raised ALP then a non-hepatic cause should be suspected such as bone disease. Alternatively, it is possible to differentiate the bone and liver isoenzymes.
· γ -GT: Alcohol and drugs such as phenytoin induce this enzyme even when there is no liver damage. It may be used to detect if patients continue to drink alcohol, but it does have a long half-life. In cholestasis it rises in parallel with the ALP.
Synthetic function
Serum proteins:
· The liver synthesises many proteins. Total protein itself is not that useful, without measuring the serum albumin level and immunoglobulin levels.
· Albumin constitutes about 65% of the total protein and as it has a short halflife of about 3 weeks, it is a good marker of synthetic function. It falls in both acute and chronic liver disease, although levels may be normal early in the disease. Low albumin levels (hypoalbuminaemia) may lead to the development of ascites and oedema. Other causes of hypoalbuminaemia include gastrointestinal losses or heavy proteinuria.
· Serum immunoglobulins are often non-specifically raised in liver disease. IgM is particularly raised in primary biliary cirrhosis, whereas IgG is raised in autoimmune hepatitis.
Prothrombin time (PT): Most clotting factors are synthesised by the liver. They have a much shorter half-life than albumin, and a prolonged PT may occur in both acute and chronic liver disease.
Vitamin K deficiency including that caused by obstructive jaundice (due to reduced absorption from the intestine) causes a prolonged PT. Parenteral replacement of vitamin K should lead to improvement of the prolonged PT within a few days if hepatic synthetic function is intact.
Related Topics