Chapter: Surgical Pathology Dissection : The Female Genital System
Placentas : Surgical Pathology Dissection
Placentas
Placentas
are submitted for evaluation because of maternal conditions, fetal/neonatalcondi-tions,
or gross anomalies of the placenta and in all multiple gestations. Many
abnormalities can be recognized with a thorough gross examina-tion. Approach
each placenta by systematically evaluating the three main components: the fetal
membranes, the umbilical cord, and the placen-tal disk.
Placentas
should initially be examined in the fresh, unfixed state. Choose a work area
that allows for the drainage of blood and fluid, which is copiously expressed
from the placental bed on sectioning. Always be aware of the clinical his-tory
before proceeding, and check the contents of the container in which the
placenta was received for any separate blood clots. Orient the placenta by
placing the spongy, red maternal surface face down and the shiny, membranous
fetal surface with umbilical cord face up. Invert the mem-branes, if necessary,
so that they are draped around the fetal surface.
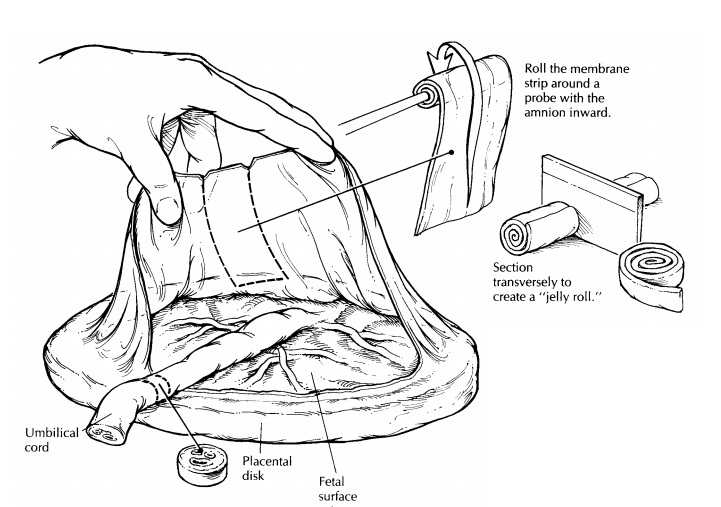
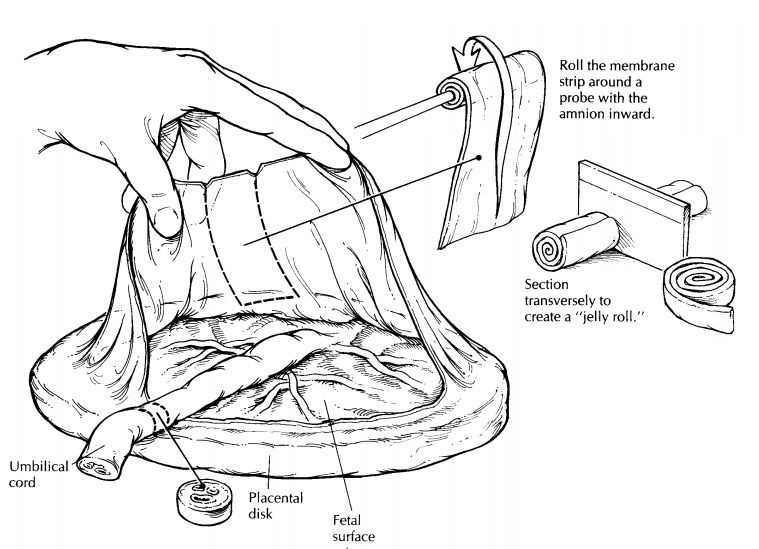
Begin
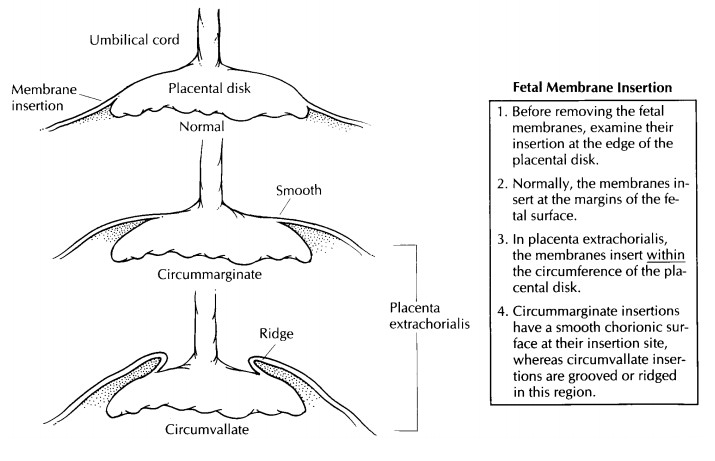
your examination with the fetal mem-branes, noting their color, lucency, and
insertion. Normal membranes should be shiny and clear and should insert at the
edge of the placental disk. Look for any opacities, which may indicate
inflammation; small white nodules, which indi-cate amnion nodosum; and meconium
staining, which may indicate intrauterine fetal hypoxia. As illustrated,
membrane insertion within the cir-cumference of the fetal surface is called
placentaextrachorialis and can be subdivided into either circummarginate (a
smooth chorionic surface at the insertion) or circumvallate (a grooved or
ridged chorionic surface at the insertion). Both may reflect previous bleeding
from earlier pla-cental separation. Next, re-create the gestational sac by
gently lifting the membranes, and cut a 2- to 3-cm-wide strip of membrane from
the ruptured margin to the placental margin. Begin-ning at the ruptured end,
roll the membrane strip with the amnion inward around a small probe. Remove the
probe, and cut the newly created ‘‘membrane roll’’ transversely for histologic
exam-ination. The membranes can now be removed by trimming them along the
placental margin.
The
umbilical cord is examined next. Record its length and site of insertion.
Although the length provided may be artificially shortened if a seg-ment was
removed in the delivery room, exces-sively short (less than 30 cm) or long
(more than 70 cm) cords are significant because of their asso-ciation with
abnormal fetal development and activity. Insertions at the edge of the placenta
or in the membranes may be associated with exposed vessels, which should be
examined carefully for any tears or thrombi. Remove the umbilical cord at its
insertion, and examine the entire length of the cord for thinning, thrombi, or
knots. True knots can be undone when the umbilical cord ends are freed, whereas
false knots cannot. Make several transverse cuts along the cord, and examine
the vessels. There should be two small thick-walled arteries and one large
thin-walled vein. At the insertion site, many vessels join together and they
may not be fused into their terminal vessel until just above this point. Also,
twisted regions of the umbilical cord can give the artificial appearance of an
increased number of vessels on cross section. Therefore, for an accurate
documentation of the number of vessels, it is best to submit a transverse
section of the umbilical cord for examination from an area that is not
excessively twisted and at least 1 cm above the insertion site.
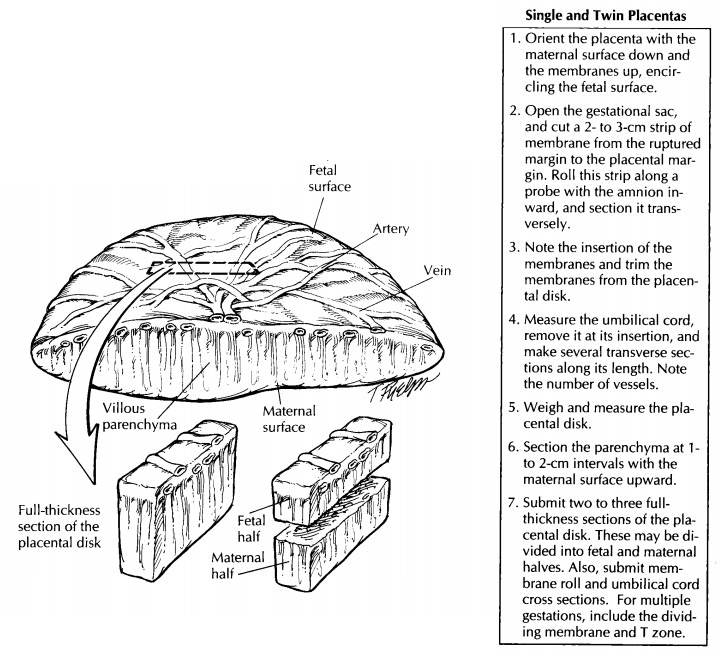
The
placenta should now be a solitary disk. Record its weight and three-dimensional
mea-surement. Any unusual shapes or extra lobes should be noted. Examine the
membranes on the fetal surface first, and look for nodules within or just below
the amnion/chorion layer. Superfi-cial white nodules or fine granularity may
repre-sent amnion nodosum, whereas firm, yellowish nodules beneath the
membranes may represent subchorionic fibrin deposition. If present, these
Next, exam-ine the vessels that radiate toward the
umbilical cord, and look for tears or thrombi. Turn the pla-centa over, and
examine the maternal surface. The cotyledons should be relatively uniform and
intact. Look for any evidence of disruption or indentation of the parenchyma.
Adherent clots without underlying compression do not neces-sarily signify a
placental abruption. Serially sec-tion the placenta at 1- to 2-cm intervals
with the maternal surface upward, and examine the pa-renchyma. The greatest
thickness of the placenta from the fetal to the maternal surface should be
measured. Look for infarcts, intervillous thrombi, or tumors. Both infarcts and
intervil-lous thrombi can appear yellow or white. Inter-villous thrombi are
usually smooth and displace the villous parenchyma, whereas infarcts involve
the villous tissue and appear more granular. If an infarct is identified, be
sure to specify the per-centage of parenchyma that is involved. Tumors are rare
in the placenta, but hemangiomas, chorio-carcinomas, and metastatic cancers can
be found.
Sections
should include the full thickness of the placenta from the central regions,
rather than from the margins. If the section is too thick to fit into one
tissue cassette, it may be divided into maternal and fetal halves. Standard
sections in-clude two central sections from different coty-ledons and any focal
lesions.
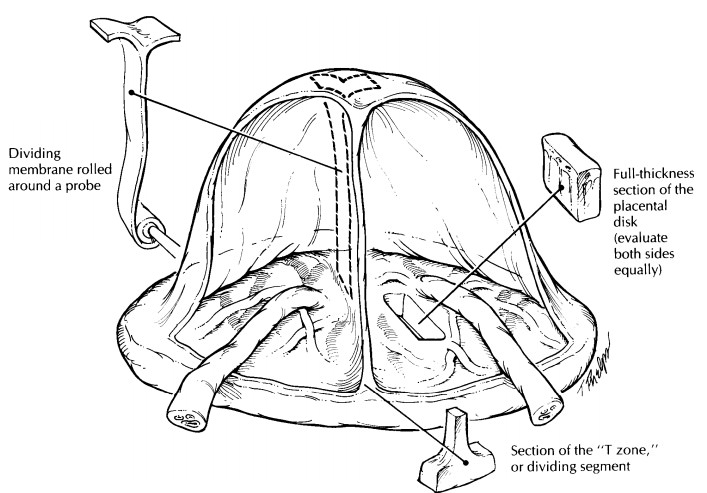
Fused
placentas from multiple gestations can be evaluated in a similar manner to
single gestations. Additional handling includes an ex-amination of the dividing
membranes and the identification of any vascular anastomoses. Di-viding
membranes are composed of two outer amnions and either one or two intervening
cho-rions. All monochorionic placentas come from monozygotic (identical) twins,
whereas dichori-onic placentas may belong to either monozy-gotic or dizygotic
(fraternal) twins. The dividing membrane can be easily peeled apart in
mono-chorionic placentas. Dichorionic placentas are moreopaque and difficult to
separate. Although you can perform this separation yourself, his-tologic
verification is necessary, and a mem-brane roll should be submitted from a
region that has not been separated. A section from the ‘‘T zone,’’ where the
membranes attach to the fetal surface, may also be submitted. Look for any
vascular anastomoses between the two sides. Note whether these are
artery-to-artery (AA), vein-to-vein (VV), or artery-to-vein (AV). Arteries can
be readily recognized by the fact that they lie on top of the veins. Abnormal
anastomoses may be reflected by one side being severely con-gested and large,
with the other being pale and small.![]()
Important Issues to Address in Your Surgical Pathology Report on Placentas
· What
procedure was performed (was the placenta removed via spontaneous delivery or
manually), and what structures/organs are present?
· What is
the trimester maturation of the villi (second or third trimester)?
· Are any
abnormalities of the placental shape, membrane insertion, or cord insertion
present?
· Are any
anomalous vessels or vessels with thrombi present?
· Is a
normal three-vessel cord present?
· Is there
inflammation of the membranes, um-bilical cord, or chorionic villi?
· Are the
maternal cotyledons disrupted, or is there compression by hematomas?
· Does the
parenchyma show any infarction? If so, what percentage is involved?
· Are any
villous thrombi or neoplasms identi-fied in the parenchyma?
· In twin
gestations, is a dividing membrane present? If so, is it
diamniotic–monochorionic or diamniotic–dichorionic?
Related Topics