Chapter: Surgical Pathology Dissection : The Female Genital System
Ovary and Fallopian Tube : Surgical Pathology Dissection
Ovary and Fallopian Tube
Ovarian Biopsies and Wedge Resections
Biopsies
and wedge resections of the ovary are infrequently performed procedures that
are used primarily for the evaluation of infertility. Biop-sies should be
measured, briefly described as to color and texture, and submitted in their
entirety. Wedge resections should also be weighed and evaluated for capsule
thickening, ‘‘powder burns’’ of endometriosis, subcortical cysts, and yellow
stromal nodularity indicating hyperthe-cosis. Sections should be taken
perpendicular to the ovarian surface to demonstrate the rela-tionship of the
capsule, cortex, and medulla.
Salpingectomies
Fallopian
tubes can be removed in part or in total. Partial salpingectomies are commonly
performed for tubal sterilization. Total salpingectomies are performed for
ectopic pregnancies, in conjunc-tion with an oophorectomy, or as part of a
hyster-ectomy specimen. Salpingectomies for primary neoplasms of the fallopian
tube are uncommon.
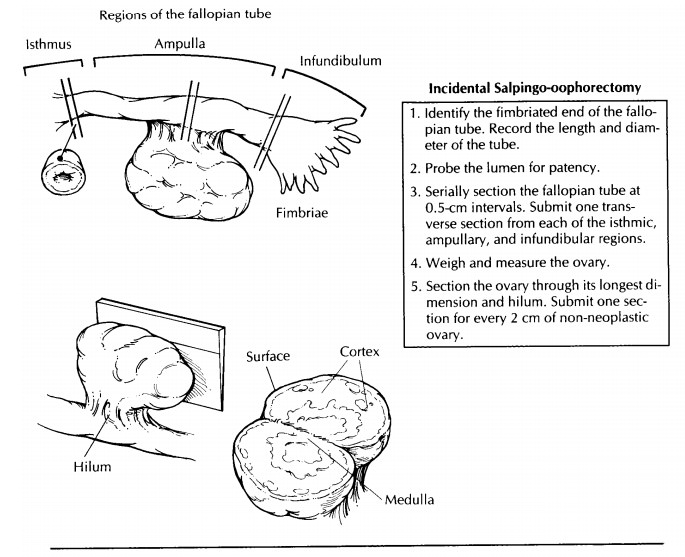
The
evaluation of the incidental salpingectomy specimen is straightforward. The
gross appear-ance of the tube is usually unremarkable. Record the length,
diameter, and color of the tube. De-scribe any features in relationship to the
different portions of the fallopian tube. The intramural portion lies within
the uterus and is not seen in separate salpingectomies. The isthmic portion is
the first 2 to 3 cm external to the uterus. The ampullary portion is the next 5
to 8 cm, and the infundibulum starts where the tube begins to widen and
encompasses the fimbriated end. The patency of the lumen may be tested with a
blunt-tipped probe. Serially section the fallopian tube at 0.5-cm intervals,
and examine it for nodularity, cysts, or masses. Submit one transverse section
from each region.
Small
segments of intervening fallopian tube are usually submitted in tubal
sterilizaton pro-cedures. For legal purposes, a complete cross section of each fallopian tube must be
micro-scopically documented.
Salpingectomies
for ectopic pregnancy should be examined for signs of rupture. Serially section
the fallopian tube, and submit any tissue with the gross appearance of products
of conception. Be sure to include the adjacent wall. If no prod-ucts of
conception are grossly identified, submit several sections from the wall in
regions of hem-orrhage as well as several from the intraluminal clot. In
contrast to uterine products of conception, in which villi are seldom seen
within the blood clots, villi are often identified in the clots from ectopic
pregnancies. Sections of uninvolved fallo-pian tube should also be submitted to
look for evidence of tubal disease contributing to the occurrence of an ectopic
pregnancy (e.g., chronic salpingitis, endometriosis, or salpingitis isth-mica nodosa).
A
salpingectomy for tubal carcinoma should be evaluated in the same manner as an
incidental salpingectomy. In addition, the size, location, and extent of the
tumor should be documented. The maximum depth of tumor penetration can be
evaluated with full-thickness transverse sections of the tube. Margins include
the cut edge of the broad ligament and the proximal fallopian tube end, if not
submitted with the uterus. In the case of a fused tubo-ovarian mass, the
primary site is almost always assumed to be the ovary.
Ovarian Cystectomies and Oophorectomies
Ovarian
cystectomies and oophorectomies are evaluated in a similar manner.
Oophorectomies may be accompanied by the fallopian tube or may be part of a
total hysterectomy specimen. A portion of broad ligament may also be present as
the ovary attaches to the posterior surface of the broad ligament and lies
inferior to the fallo-pian tube.
Incidental
oophorectomies are easily handled. Record the weight and dimensions of the
ovary. Examine the outer surface for cysts, nodules, or adhesions. Bivalve the
ovary with a cut through its longest dimension and midhilum. Evaluate the
sectioned surface for any cysts or nodules, and designate their location as
either cortical, medullary, or hilar. Keep in mind that the ap-pearance of the
ovary will vary considerably with the age and the reproductive status of the
woman. The normal ovary in the reproductive years can measure up to 4 cm,
whereas an ovary this size in a postmenopausal woman warrants close evaluation.
Submit one section for every 2 cm of non-neoplastic ovary. If the ovary and
fallopian tube were removed as a prophylactic procedure in a woman with a
family history of ovarian or breast carcinoma, the entire ovary and fallopian
tube should be submitted.
Cystectomies
are usually performed for benign lesions or in women with ovarian masses who
wish to preserve their fertility. The most common indication is for the removal
of a dermoid cyst. After weighing and measuring the cyst, examine the external
surface for evidence of rupture. Place the cyst in a container, and carefully
make a small incision in the wall to allow its contents to be drained. Note the
color and consistency of the cyst fluid. Continue the incision with a pair of
scissors to expose the entire inner surface. The thick sebaceous fluid within a
dermoid cyst may have to be removed by rinsing briefly with hot water. Examine
the cyst lining, and look for any regions of granularity or papillary
projections. In dermoid cysts, look for Rokitansky’s tubercle, which appears as
a firm, nodular excrescence. This region and any other thickened areas should
be submitted in their entirety to look for evidence of immature elements.
Large, unilocular cysts with a smooth inner lining may be cut in strips and
submitted like placental membrane rolls to get a maximum view of the cyst wall.
Cystectomies for lesions other than unilocular smooth-walled cysts or dermoid
cysts should be handled as described next.
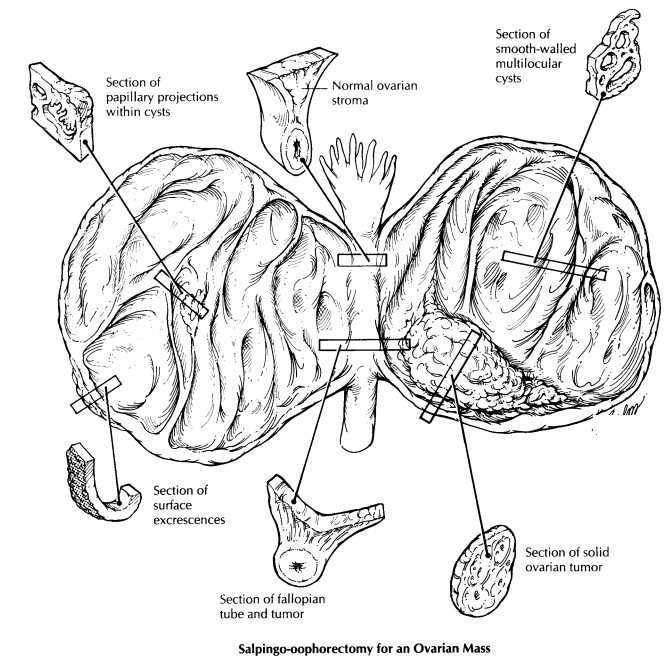
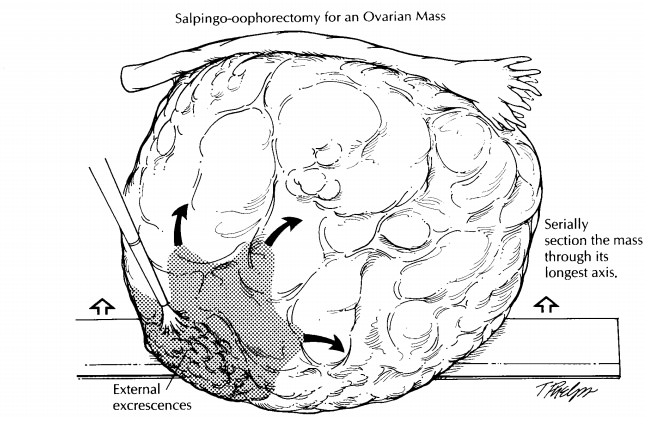
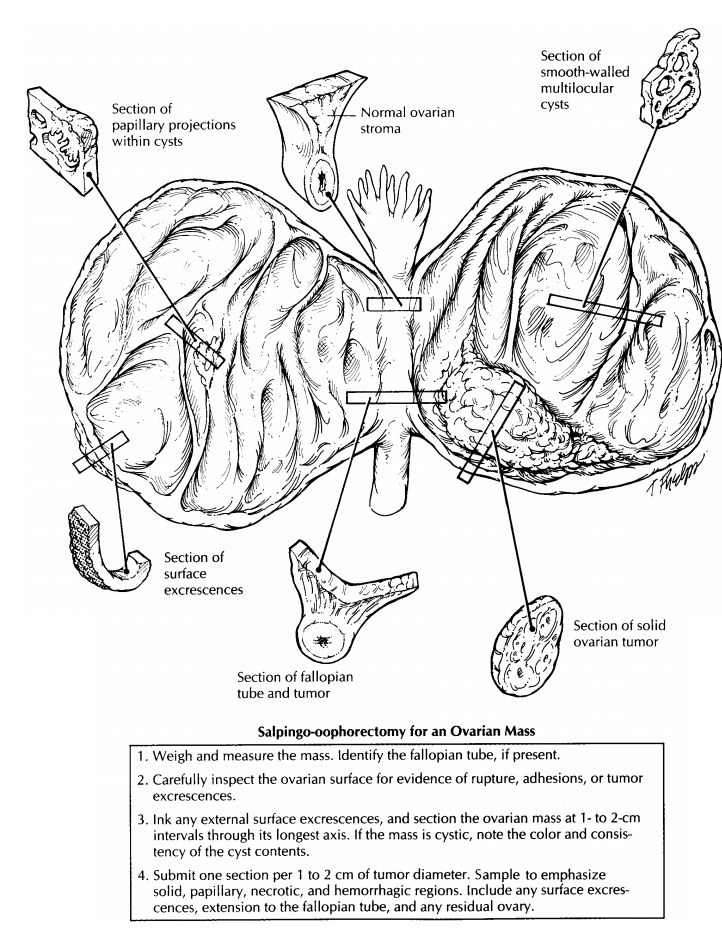
Oophorectomies
for ovarian tumors can be quite large and heavy. Often, the only recogniz-able
structure is the fallopian tube, which may be attenuated and stretched over the
ovarian sur-face. Begin by weighing and measuring the speci-men. Closely
examine the surface for evidence of rupture, adhesions, or nodular tumor excres-cences.
Ink these regions for orientation. Section the ovarian mass at 1-cm intervals
through its longest axis. If the mass is cystic, you may want to perform this
in a pan or on a work station that allows for easy drainage of fluid. Remem-ber
to document the color and consistency of the cyst fluid. Is the fluid serous,
mucinous, or hem-orrhagic? Note whether the mass is solid, cystic, or both. If
both, document the percentage of each region. Examine the surfaces of the cysts
for evi-dence of granularity, nodules, or papillary projec-tions. The thickness
of the cyst walls should also be recorded. Describe any regions of hemorrhage
or necrosis. Try to find any residual ovarian pa-renchyma. This is commonly
found in the region immediately adjacent to the fallopian tube. If a stromal or
steroid cell tumor is suspected, tis-sue should be saved frozen in case fat
stains are needed. Consider saving frozen tissue for any small, blue,
round-cell tumor, particularly if the tumor is in a pediatric patient or is predominantly
intra-abdominal. Photographs of the cut surface can aid in documentation of the
mass and for designating where sections were taken. At this point, it may be
helpful to fix the 1-cm slices in formalin before further manipulation.
Historically,
ovarian tumors are submitted with a minimum of one section per 1 to 2 cm of the
greatest tumor dimension. This rule is espe-cially useful in the case of
mucinous tumors, which tend to have only focal regions demonstrat-ing atypical
or frankly invasive elements. If the tumor is uniform throughout, as many
serous tumors are, fewer sections may be prudent. In general, sections should
be submitted from re-gions that are solid, hemorrhagic, or necrotic. Cysts that
show granular, nodular, or papillary excrescences should be thoroughly sampled.
Also be submitted in their entirety to look for evidence of immature elements.
Large, unilocular cysts with a smooth inner lining may be cut in strips and
submitted like placental membrane rolls to get a maximum view of the cyst wall.
Cystectomies for lesions other than unilocular smooth-walled cysts or dermoid
cysts should be handled as described next.
Oophorectomies
for ovarian tumors can be quite large and heavy. Often, the only recogniz-able
structure is the fallopian tube, which may be attenuated and stretched over the
ovarian sur-face. Begin by weighing and measuring the speci-men. Closely
examine the surface for evidence of rupture, adhesions, or nodular tumor
excres-cences. Ink these regions for orientation. Section the ovarian mass at
1-cm intervals through its longest axis. If the mass is cystic, you may want to
perform this in a pan or on a work station that allows for easy drainage of
fluid. Remem-ber to document the color and consistency of the cyst fluid. Is
the fluid serous, mucinous, or hem-orrhagic? Note whether the mass is solid,
cystic, or both. If both, document the percentage of each region. Examine the
surfaces of the cysts for evi-dence of granularity, nodules, or papillary
projec-tions. The thickness of the cyst walls should also be recorded. Describe
any regions of hemorrhage or necrosis. Try to find any residual ovarian
pa-renchyma. This is commonly found in the region immediately adjacent to the
fallopian tube. If a stromal or steroid cell tumor is suspected, tis-sue should
be saved frozen in case fat stains are needed. Consider saving frozen tissue
for any small, blue, round-cell tumor, particularly if the tumor is in a
pediatric patient or is predominantly intra-abdominal. Photographs of the cut
surface can aid in documentation of the mass and for designating where sections
were taken. At this point, it may be helpful to fix the 1-cm slices in formalin
before further manipulation.
Historically, ovarian tumors are submitted with a minimum of one section per 1 to 2 cm of the greatest tumor dimension. This rule is espe-cially useful in the case of mucinous tumors, which tend to have only focal regions demonstrat-ing atypical or frankly invasive elements. If the tumor is uniform throughout, as many serous tumors are, fewer sections may be prudent. In general, sections should be submitted from re-gions that are solid, hemorrhagic, or necrotic. Cysts that show granular, nodular, or papillary excrescences should be thoroughly sampled.
Also include
any regions that appear sieve-like or honeycombed. Multiple large unilocular
cysts may be more judiciously sampled. Sections that demonstrate the junction
between the ovary and adjacent fallopian tube, as well as any residual ovary,
should also be submitted.
Specimens for Ovarian Tumor Staging
The
staging procedure for an ovarian tumor can include an omentectomy, multiple
biopsies of the peritoneum, and lymph node dissections.
Omentectomy
specimens should be weighed, measured, and serially sectioned at 0.5-cm
inter-vals to look for gross tumor nodules. Measure the size of the gross tumor
and specifically indicate if it is 2 cm or less or more than 2 cm for staging
purposes. Palpate the fat for areas of induration or small miliary nodules. For
grossly visible tumor involvement, one to three representative sections should
be submitted for histology. If the tumor is not grossly visible, take multiple
sections from the firmest regions in the omental fat. Five representative
sections are usually suffi-cient, although some authorities recommend up to ten
sections.
Peritoneal
small biopsies should be routinely processed and submitted in their entirety. If
the tumor extensively involves the pelvic perito-neum, a cavitronic ultrasonic
surgical aspirator may be used to remove the implants. Tissue removed this way
can be handled like a curet-tage specimen.
A
predominant mass in the omentum or peri-toneum, with no ovarian involvement and
no tumor in the ovary invading to a depth of 5 mm or more, is generally
considered to be a primary peritoneal carcinoma.
Lymph
nodes are received separately and des-ignated by location. They can be handled
in a routine manner for evaluation of metastatic dis-ease.
Important Issues to Address in Your Surgical Pathology Report on Ovarian Tumors
· What
procedure was performed, and what structures/organs are present?
· Is a
neoplasm present? Is it of epithelial, sex-cord/stromal, germ cell, or
metastatic origin? Metastatic involvement is suggested by the presence of
multiple tumor nodules, surface implants, and vascular space involvement.
· What are
the size, histologic type, and grade of the neoplasm?
· Was the
ovarian capsule ruptured?
· Does the
tumor involve the ovarian capsule?
· Does the
tumor involve the adjacent fallopian tube or broad ligament?
· Is there
capillary–lymphatic space invasion?
· If
submitted, does the tumor involve the con-tralateral ovary and/or the serosa or
paren-chyma of the uterus? When identical tumors involve both the ovary and
endometrium, con-sider independent primary sites of origin.
· Does the
tumor involve the omentum? Is the tumor microscopic, 2 cm or less, or more than
2 cm? Consider a primary peritoneal origin if there is no or minimal ovarian
involvement.
· Does the
tumor involve any lymph nodes? In-clude the number of nodes involved and the
number of nodes examined at each specified site.
·
Do the soft tissue staging biopsies show tumor
implants? If so, specify whether they are inva-sive or noninvasive.
Related Topics