Chapter: Surgical Pathology Dissection : The Female Genital System
Hysterectomy for Endometrial Cancer
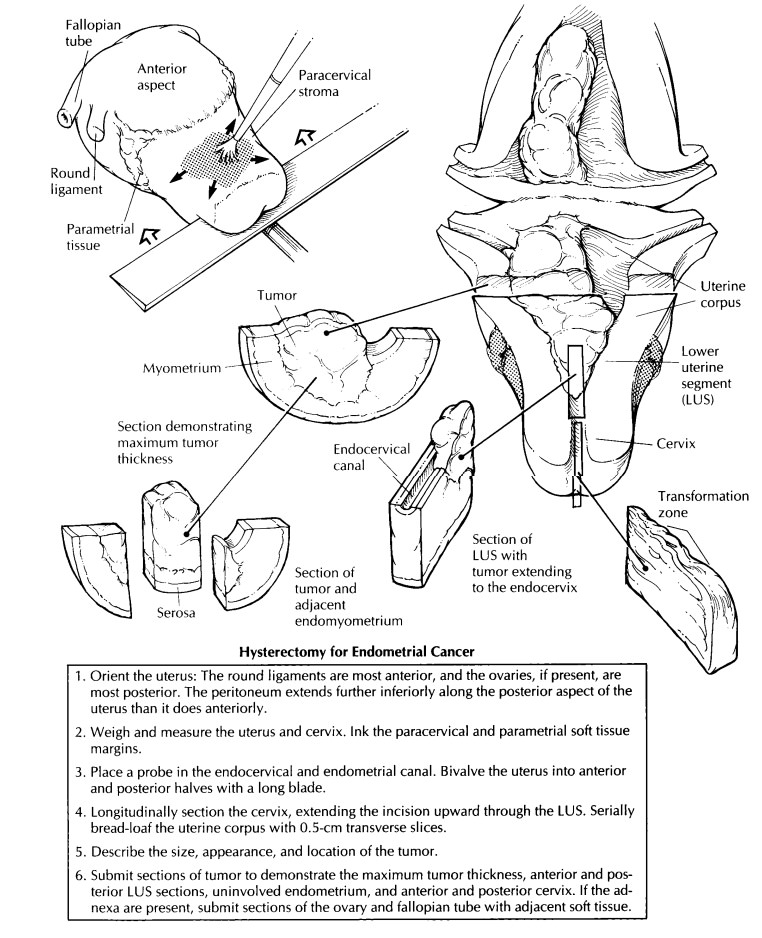
Hysterectomy for Endometrial Cancer
The
approach to hysterectomies performed for endometrial cancer parallels the
approach to hysterectomies for benign disease. Additional steps include inking
the paracervical and para-metrial soft tissue margins and evaluating the extent
of the tumor.
Orient, weigh, and measure the uterus as described in the section on hysterectomies for benign disease, and ink the soft tissue resection margins around the cervical canal. Also, ink the parametrial tissue, which extends along the body of the uterus and into the broad ligament. Care-fully examine the serosal surfaces for evidence of tumor extension. Ink these areas a different color for orientation.
If the adnexa are present, remove them at their lateral insertions
along the uterus. Make multiple transverse cuts through the ovary and fallopian
tube, looking for evidence of either direct tumor extension or metastatic
spread. Submit at least one section from each side to demonstrate the ovary and
fallopian tube with adjacent soft tissue.
Bivalve
the uterus by using a long, sharp knife guided by a probe placed through the
cervical canal. Closely examine the endometrial cavity. Endometrial carcinomas can be shaggy, sessile
tumors or polypoid masses arising from the surface of the endometrium. They may
be either focal or diffuse. The sounding depth of the uterus from the external
cervical os to the superior limit of the endometrial cavity may be measured,
but it is no longer used in the staging of endometrial cancers.
While
the tumor is fresh, remove a portion to freeze for future molecular diagnostic
tests if desired. The bivalved uterus may now be photographed and pinned to a
wax tablet for fixation.
The
dissection begins with longitudinal sectioning of the cervix. Extend these
incisions through the lower uterine segment to include both endometrial and
endocervical mucosal surfaces. Note whether or not the tumor grossly involves
the endocervical mucosa and/or stroma.
Submit a
section of this region from the anterior and posterior halves to evaluate for
tumor extension into the cervix, an important factor in determining the stage
of the cancer. This step may
also be
accomplished by taking transverse sections of the upper endocervix and lower
uterine segment. Next, serially bread-loaf the uterine corpus and lower uterine
segment with transverse sections. Record the size, location, and appearance of
the tumor. Describe the pattern of invasion. Does the tumor have a broad
pushing front, an infiltrating finger-like pattern, or is it discontinuous?
Measure the greatest depth of tumor invasion into the myometrium starting from
the normal junction of the endometrium and the myometrium. In addition, measure
the total myometrial thickness at this point, and specify the uninvolved
distance from the deep tumor/myometrial junction to the serosa. When selecting
sections for histologic analysis, include the deepest point of tumor invasion
as well as the interface with grossly uninvolved endometrium. The best sections
are those that show the full thickness from the endometrium to the serosa.
Sometimes, however, the myometrium may be too thick to fit in a standard-size
tissue cassette. In these situations, divide the section into endometrial and
serosal halves. Be sure to designate their relationship clearly in your summary
of sections.
Lymph
nodes from the pelvic and para-aortic regions may also be included as separate
specimens. They can be handled in a routine manner for evaluation of metastatic
disease.
Important Issues to Address in Your Surgical Pathology Report on Hysterectomies for Endometrial Cancer
What procedure was performed, and what structures/organs are present?
What is the size of the tumor?
What are the histologic type and grade of neoplasm present?
What is the maximum depth of tumor invasion (in millimeters)? (Measure from the
normal endometrial/myometrial junction.)
What is the total myometrial thickness at the deepest point of invasion (in
millimeters)?
What is the distance from the deepest tumor/myometrial junction to the serosa
(in millimeters)?
Does the tumor extend through the serosa?
Does the tumor involve the endocervix? (Specify surface glandular
and/or stromal involvement.)
Is capillary–lymphatic space invasion seen?
Does the tumor involve the adjacent adnexa?
Does the tumor involve any margins (cervical/vaginal, right
paracervical/parametrial, left paracervical/parametrial)? Give the
distance of the tumor from closest margin (in centimeters).
Does the tumor involve any lymph nodes? (Include the number of nodes involved
and the number of nodes examined at each specified site.)
Related Topics