Chapter: Essentials of Psychiatry: Mental Disorders Due to a General Medical Condition
Personality Change Due to a General Medical Condition
Personality Change Due to a
General Medical Condition
Definition
The personality of an adult represents a coalescence of various personality traits present in childhood and adolescence, and is generally quite enduring and resistant to change. Thus, the ap-pearance of a significant change in an adult’s personality is an ominous clinical sign and indicates the presence of intracranial pathology. Patients themselves may not be aware of the change, however to others, who have known the patient over time, the change is often quite obvious: such observers often note that the patient is “not himself” anymore.
In most cases, the change is nonspecific in nature:
there may be either a gross exaggeration of hitherto minor aspects of the
patient’s personality or the appearance of a personality trait quite
uncharacteristic for the patient. Traits commonly seen in a personality change,
as noted in DSM-IV-TR, include lability, disinhibition, aggressiveness, apathy,
or suspiciousness.
In addition to these nonspecific changes, there are
two specific syndromes which, though not listed in DSM-IV-TR, are
well-described in the literature, namely, the frontal lobe syn-drome and the
interictal personality syndrome (also known as the “Geschwind syndrome”).
The frontal
lobe syndrome is characterized by a variable mixture of disinhibition,
affective changes, perseveration and abulia. Disinhibition manifests with an
overall coarsening of be-havior. Attention to manners and social nuances is
lost: patients may eat with gluttony, make coarse and crude jokes, and may
engage in unwelcome and inappropriate sexual behavior, perhaps by
propositioning much younger individuals or masturbating in public. Affective
changes tend toward a silly, noninfectious euphoria; depression, however, may
also be seen. Perseveration presents with a tendency to persist in whatever
task is currently at hand, and patients may repeatedly button and unbutton
cloth-ing, open and close a drawer or ask the same question again and again.
Abulia is characterized by an absence of desires, urges or interests, and such
patients, being undisturbed by such phenom-ena, may be content to sit placidly
for indefinite periods of time. Importantly, such abulic patients are not
depressed, nor are they incapable of activity: indeed, with active supervision
they may be able to complete tasks; however, once supervision stops, so too do
the patients, as they lapse back into quietude.
The interictal
personality syndrome, a controversial entity (Bear et al., 1982; Rodin and Schmaltz, 1984) is said to occur as a
complication of longstanding uncontrolled epilepsy, with repeated grand mal or
complex partial seizures. The cardi-nal characteristic of this syndrome is what
is known as “viscos-ity”, or, somewhat more colloquially, “stickiness”. Here,
patients seem unable to let go or diverge from the current emotion or train of
thought: existing affects persist long after the situation which occasioned
them, and a given train of thought tends to extend itself indefinitely into a
long-winded and verbose circum-stantiality or tangentiality. This viscosity of
thought may also appear in written expression as patients display
“hypergraphia”, producing long and rambling letters or diaries. The inability
to “let go” may even extend to such simple acts as shaking hands, such that
others may literally have to extract their hand to end the handshake. The
content of the patient’s viscous speech and writing generally also changes, and
tends toward mystical or abstruse philosophical speculations. Finally, there is
also a tendency to hyposexuality, with an overall decrease in libido (Blumer,
1970).
Etiology and Pathophysiology
A personality change is not uncommonly seen as the
prodrome to schizophrenia, however in such cases the eventual appearance of the
typical psychosis will indicate the correct diagnosis.
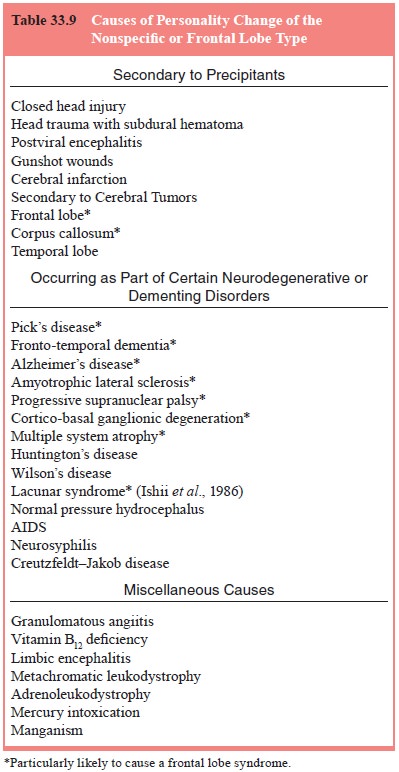
Personality change of the nonspecific or of the
frontal lobe type, as noted in Table 33.9, may occur secondary to precipi-tants (e.g., closed head injury), secondary to cerebral tumors (especially
those of the frontal or temporal lobes) or as
part of certain neurodegenerative or
dementing disorders. Finally, there
is a group of miscellaneous causes.
In Table 33.9, those dis-orders or diseases which are particularly prone to
cause a person-ality change of the frontal lobe type are indicated by an
asterisk. The interictal personality syndrome occurs only in the setting of
chronic repeated grand mal or complex partial seizures, and may represent
microanatomic changes in the limbic system which have been “kindled” by the
repeated seizures (Adamec and Stark-Adamec,1983;Bear,1979)
In the case of personality change occurring secondary to precipitants, the etiology is fairly obvious; an exception might be cerebral infarction, but here
the acute onset and the presence of “neighborhood” symptoms are suggestive. In
ad-dition to infarction of the frontal lobe, personality change has also been
noted with infarction of the caudate nucleus and of the thalamus.
In the case of personality change occurring secondary to precipitants, the etiology is fairly obvious; an exception might be cerebral infarction, but here
the acute onset and the presence of “neighborhood” symptoms are suggestive. In
ad-dition to infarction of the frontal lobe, personality change has also been
noted with infarction of the caudate nucleus and of the thalamus.
Personality change occurring secondary to cerebral tumors
may not be accompanied by any distinctive features, and indeed a personality change may be the only clinical evidence of a
tumor for a prolonged period of time.
Personality change occurring as part of certain neuro-degenerative or dementing disorders deserves
special men-tion, for in many instances the underlying disorder may present
with a personality change; this is particularly the case with Pick’s disease,
fronto-temporal dementia and Alzheimer’s disease. The inclusion of amyotrophic
lateral sclerosis here may be surpris-ing to some, but it is very clear that,
albeit in a small minority cerebral symptoms may not only dominate the early
course of ALS, but may even constitute the presentation of the disease. In the
case of the other neurodegenerative disorders (i.e., progres-sive supranuclear
palsy, cortico–basal ganglionic degeneration, multiple system atrophy,
Huntington’s disease and Wilson’s dis-ease) a personality change, if present,
is typically accompanied by abnormal involuntary movements of one sort or
other, such as parkinsonism, ataxia or chorea. The lacunar syndrome, oc-curring
secondary to multiple lacunar infarctions affecting the thalamus, internal
capsule or basal ganglia, deserves special mention as it very commonly causes a
personality change of the frontal lobe type by interrupting the connections
between the thalamus or basal ganglia and the frontal lobe. Normal pres-sure
hydrocephalus is an important diagnosis to keep in mind, as the condition is
treatable: other suggestive symptoms include a broad-based shuffling gait and
urinary urgency or incontinence. AIDS should be suspected whenever a
personality change is accompanied by clinical phenomena suggestive of immunode-ficiency,
such as thrush. Neurosyphilis may present with a per-sonality change
characterized by slovenliness and disinhibition. Creutzfeldt–Jakob disease may
also present with a personality change, and this appears particularly likely
with the “new vari-ant” type: the eventual appearance of myoclonus suggests the
correct diagnosis.
The miscellaneous
causes represent the diagnostic “ze-bras” in the differential for
personality change. Of them two de-serve comment, given their treatability:
granulomatous angiitis is suggested by prominent headache, and vitamin B12
deficiency by the presence of macrocytosis or a sensory polyneuropathy.
Assessment and Differential Diagnosis
Personality change must be clearly distinguished
from a per-sonality disorder. The personality disorders (e.g., antisocial
personality disorder, borderline personality disorder), all dis-cussed
elsewhere in this book, do not represent a change in the patient’s personality
but rather have been present in a lifelong fashion. In gathering a history on a
patient with a personal-ity change, one finds a more or less distinct time when
the “change” occurred; by contrast, in evaluating a patient with a personality
disorder, one can trace the personality traits in question in a more or less seamless
fashion back into adoles-cence, or earlier.
The frontal lobe syndrome, at times, may present
further diagnostic questions, raising the possibility of either mania, when
euphoria is prominent, or depression, when abulia is at the forefront. Mania is
distinguished by the quality of the euphoria, which tends to be full and
infectious in contrast with the silly, shallow and noninfectious euphoria of
the frontal lobe syndrome. Depression may be distinguished by the quality of
the patients’ experience: depressed patients definitely feel something, whether
it be a depressed mood or simply a weighty sense of oppression. By contrast,
the patient with abulia generally feels nothing: the “mental horizon” is clear
and undisturbed by any dysphoria or unpleasantness.
MRI scanning is diagnostic in most cases: where
this is uninformative, further testing is dictated by one’s clinical
suspi-cions (e.g., HIV testing).
The interictal personality syndrome must be
distin-guished from a personality change occurring secondary to a slowly
growing tumor of the temporal lobe. In some cases, very small tumors, which may
escape detection by routine MRI scanning, may cause epilepsy, and then, with
continued growth, also cause a personality change. Thus, in the case of a
patient with epilepsy who develops a personality change, the diagnosis of the
interictal personality syndrome should not be made until a tumor has been ruled
out by repeat MRI scanning.
Epidemiology and Comorbidity
Personality change is common, and is seen with especial
fre-quency after closed head injury and as a prodrome to the de-mentia
occurring with such neurodegenerative disorders as Pick’s disease,
fronto-temporal dementia and Alzheimer’s disease.
Course
This is determined by the underlying cause; in the
case of the interictal personality syndrome it appears that symptoms persist
even if seizure control is obtained.
Treatment
Treatment, if possible, is directed at the
underlying cause. Mood stabilizers (i.e., lithium, carbamazepine or divalproex)
may be helpful for lability, impulsivity and irritability; propranoalol, in
high dose, may also have some effect on irritability. Neurolep-tics (e.g.,
olanzapine, risperidone, haloperidol) may be helpful when suspiciousness or
disinhibition are prominent. Antide-pressants (e.g., an SSRI) may relieve
depressive symptoms. Regardless of which agent is chosen, it is prudent, given
the general medical condition of many of these patients, to “start low and go
slow”. In many cases, some degree of supervision will be required.
Related Topics