Chapter: Essentials of Psychiatry: Mental Disorders Due to a General Medical Condition
Mood Disorder with Manic Features
Mood Disorder with Manic Features
Definition
Mood disorder due to a general medical condition
with manic features is characterized by a prominent and persistently ele-vated,
expansive or irritable mood which, on the basis of the his-tory, physical or
laboratory examinations can be attributed to an underlying general medical condition.
Other manic symptoms, such as increased energy, decreased need for sleep,
hyperactivity, distractibility, pressured speech and flight of ideas, may or
may not be present.
Etiology and Pathophysiology
The vast majority of cases of sustained, elevated
or irritable mood occur as part of four primary disorders, namely bipolar I
disorder, bipolar II disorder, cyclothymic disorder and schizoaf-fective
disorder (bipolar type). Cases of elevated or irritable mood secondary to other
causes (e.g., secondary to treatment with corticosteroids) are much less
common. Table 33.4 lists sec-ondary causes of elevated or irritable mood, with
these causes divided into categories designed to facilitate the task of
differ-ential diagnosis.
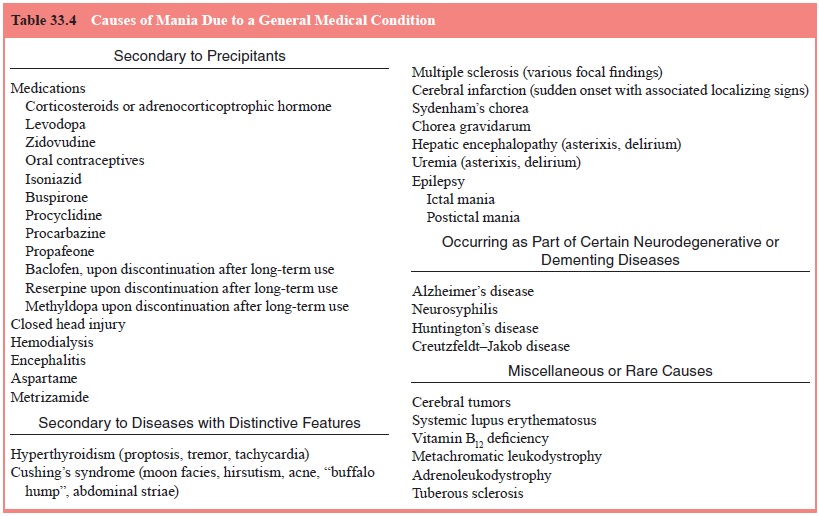
In utilizing Table 33.4, the first step is to
determine whether the mania could be secondary
to precipitants. Sub-stance-induced mood disorder related to drugs of abuse
is covered in the relevant substance-related disorders. Of the precipitating
factors listed in Table 33.4, medications are the most common offenders.
Before, however, attributing the mania to one of these medications, it is
critical to demonstrate that the mania occurred only after initiation of that
medication; ideally, one would also want to show that themania spontaneously
resolved subsequent to the medication’s discontinuation. Of the medications
listed, corticosteroids, such as prednisone, are likely to cause mania, with
the likelihood in-creasing in direct proportion to dose: in one study
(Wolkow-itz et al., 1990), 80 mg of
prednisone produced mania within five days in 75% of subjects. Levodopa is the
next most likely cause, and in the case of levodopa the induced mania may be so
pleasurable that some patients have ended up abusing the drug (Giovannoni et al., 2000). Anabolic steroid abuse
may cause an irritable mania, and such a syndrome occurring in a “bulked up”
patients should prompt a search for other clinical evidence of abuse, such as
gynecomastia and testicular atrophy. Closed head injury may be followed by mania
either directly upon emergence from postcoma delirium, or after an interval of
months. Hemodialysis may cause mania, and in one case (Jack et al., 1983) mania occurred as the
presenting sign of an even-tual dialysis dementia. Encephalitis may cause mania,
as, for example, in postinfectious encephalomyelitis, with the correct
diagnosis eventually being suggested by more typical signs such as delirium or
seizures. Encephalitis lethargica (Von Economo’s disease; European Sleeping
Sickness) may also be at fault, with the diagnosis suggested by classic signs
such as sleep reversal or oculomotor paralyses.
Mania occurring secondary to disease with distinctive features is immediately suggested by these features, as listed in Table 33.4. Some elaboration may be
in order regarding ma-nia secondary to cerebral infarction. This cause, of
course, is suggested by the sudden onset of the clinical disturbance, with the
mania being accompanied by various other more or less localizing signs: what is
most remarkable here is the variety of structures which, if infarcted, may be
followed by mania
Thus, mania has been noted with infarction of the
midbrain, thalamus (either on the right side or bilaterally, anterior limb of
the internal capsule and adjacent caudate on the right, and subcortical white
matter or cortical infarction on the right in the frontoparietal or temporal
areas. Mania associated with epilepsy may also deserve additional comment.
Ictal mania is characterized by its paroxysmal onset, over seconds and the diagnosis
of postictal mania is suggested when mania oc-curs shortly after a “flurry” of
grand mal or complex partial seizures.
Mania occurring
as part of certain neurodegenerative or
dementing diseases is suggested, in general, by a concur-rent dementia, and
in most cases the mania plays only a minor role in the overall clinical
pictures. Neurosyphilis, however, is an exception to this rule, for in patients
with general paresis of the insane (dementia paralytica) mania may dominate the
picture.
Of the miscellaneous
or rare causes of mania, cerebral tumors are the most important to keep in
mind, with mania be-ing noted with tumors of the midbrain, tumors compressing
the hypothalamus, e.g., a craniopharyngioma or a pituitary adenoma, and tumors
of the right thalamus, right cingulate gyrus or one or both frontal lobes.
Assessment and Differential Diagnosis
In most cases of mania secondary to precipitants, the cause (e.g., treatment with high
dose prednisone) is fairly straightforward; in cases secondary to diseases with distinctive features or occurring as
part of certain neurodegenerative or dementing diseases, the cause is
generally readily discernible if the
clinician is alert to the telltale distinctive features (e.g., a Cushingoid
habitus) and to the presence of dementia indicat-ing one of the dementing
disorders listed in Table 33.4. The miscellaneous
or rare causes represent the “zebras” in the dif-ferential of secondary
mania, and are generally only resorted to when other investigations prove
unrewarding.
As a rule, it is very rare for mania to constitute
the initial presentation of any of the disease or disorders listed in Table
33.4; thus, other evidence of their presence will become evident dur-ing the
routine history and physical examination. Exceptions to the rule include
neurosyphilis, vitamin B12 deficiency and Creutzfeldt–Jakob disease,
however in all these cases continued observation will eventually disclose the
appearance of other evi-dence suggestive of the correct diagnosis.
It must always be kept in mind that certain
medications (e.g., antidepressants) may precipitate mania in patients with
bi-polar disorder: in such cases, history will reveal earlier episodes of
either depression, or mania, or both and such cases of mania should not be
considered secondary.
Epidemiology and comorbidity
Relative to cases of primary mania (e.g., bipolar
disorder), sec-ondary mania is relatively rare. In certain settings, however,
sec-ondary mania may be so common as to merit a “top” position on the differential
diagnosis; a prime example would be when prednisone is used in high doses, as
in the treatment of multiple sclerosis or rheumatoid arthritis.
Course
Most cases of medication-induced mania begin to
clear in a mat-ter of days; for other causes, the course of the mania generally
reflects the course of the underlying disease.
Treatment
Treatment, if possible, is directed at the underlying cause. In cases where such etiologic treatment is not possible, or not rapidly ef-fective enough, pharmacologic measures are in order. Mood sta-bilizers, such as lithium or divalproex used in a fashion similar to that for the treatment of mania occurring in bipolar disorder, are commonly used: both lithium and divalproex are effective in the prophylaxis of mania occurring secondary to prednisone; case reports also support the use of lithium for mania secondary to zidovudine and divalproex for mania secondary to closed head injury. As between lithium and divalproex, in cases where there is a risk for seizures (e.g., head injury, encephalitis, stroke or tu-mors), divalproex clearly is preferable
In cases where emergent treatment is required,
before lith-ium or divalproex could have a chance to become effective, oral or
intramuscular lorazepam or haloperidol (in doses of 2 mg and 5 mg,
respectively) may be utilized, again much as in the treat-ment of mania in
bipolar disorder.
Related Topics