Chapter: Essentials of Psychiatry: Mental Disorders Due to a General Medical Condition
Mood Disorder with Obsessive–Compulsive Symptoms
Mood Disorder with
Obsessive–Compulsive Symptoms
Definition
Obsessions consist of unwanted, and generally
anxiety-provoking, thoughts, images or ideas which repeatedly come to mind
despite patients’ attempts to stop them. Allied to this are compulsions, which
consist of anxious urges to do or undo things, urges which, if resisted, are
followed by rapidly increasing anxiety which can often only be relieved by
giving into the compulsion to act. The acts themselves which the patients feel
compelled to perform are often linked to an apprehension on the patients’ part
that they have done something that they ought not to have done or have left
undone something which they ought to have done. Thus, one may feel compelled
repeatedly to subject the hands to washing to be sure that all germs have been
removed, or repeatedly to go back and check on the gas to be sure that it had
been turned off.
Etiology and Pathophysiology
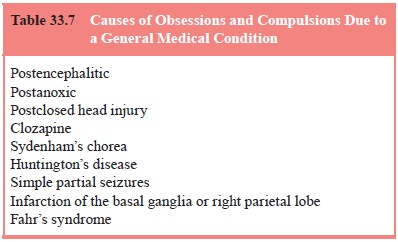
In the vast majority of cases, obsessions and
compulsions oc-cur as part of certain primary psychiatric disorders, including
obsessive–compulsive disorder, depression, schizophrenia and Tourette’s
syndrome. Those rare instances where obsessions and compulsions are secondary
to a general medical condition or medication are listed in Table 33.7.
In most cases, these causes of secondary obsessions
or compulsions are readily discerned, as for example, a history of
encephalitis, anoxia, closed head injury or treatment with clozap-ine.
Sydenham’s chorea is immediately suggested by the appear-ance of chorea,
however, it must be borne in mind that obsessions and compulsions may
constitute the presentation of Sydenham’s chorea, with the appearance of chorea
being delayed for days
(Swedo et al.,
1989). Ictal obsessions or compulsions, constitut-ing the sole clinical
manifestation of a simple partial seizure, may, in themselves, be
indistinguishable from the obsessions and compulsions seen in
obsessive–compulsive disorder, but are sug-gested by a history of other seizure
types, for example, complex partial or grand mal seizures. Infarction of the
basal ganglia or parietal lobe is suggested by the subacute onset of obsessions
or compulsions accompanied by “neighborhood” symptoms such as abnormal
movements or unilateral sensory changes. Fahr’s syn-drome, unlike the
foregoing, may be an elusive diagnosis, only suggested perhaps when CT imaging
incidentally reveals calcifi-cation of the basal ganglia.
Assessment and Differential Diagnosis
Most causes of secondary obsessions and compulsions
are picked up on the routine history and physical examination, with the
pos-sible exception of ictal cases, and here it is critical to make a close
inquiry as to a history of other seizure types: ictal EEGs are not reliable
here, as they are often normal in the case of simple partial seizures. In
doubtful cases a “diagnosis by treatment response” to a trial of an
anticonvulsant may be appropriate.
Epidemiology and Comorbidity
As noted earlier, secondary obsessions and
compulsions are rela-tively rare.
Course
Although the course of obsessions and compulsions
due to fixed lesions, such as those seen with head trauma or cerebral
infarc-tion tends to be chronic, some spontaneous recovery may be an-ticipated
over the following months to a year.
Treatment
When treatment of the underlying cause is not
possible, a trial of an SSRI, as used for obsessive–compulsive disorder, might
be appropriate.
Related Topics