Chapter: Paediatrics: Neonatology
Paediatrics: Necrotizing enterocolitis
Necrotizing enterocolitis
Incidence
The most common neonatal surgical
emergency. Incidence 1‚Äď3/1000 live births (5‚Äď10% in VLBW infants). Incidence is
reduced 6-fold in preterm infants fed breast milk. Typically a sporadic
condition affecting preterm infants (790% of cases), but can be epidemic or
occur in term infants. The disease may just involve an isolated area of gut, or
be extensive. Distal ter-minal ileum and proximal colon are most frequently
affected. Multi-organ failure is associated with diffuse disease.
Cause
Multifactorial. Severe intestinal
necrosis is end result of an exaggerated immune response within the immature
bowel leading to inflammation and tissue injury. NEC rarely occurs before milk
feeding commences, but tim-ing of first feed appears not to be relevant.
Predisposing factors:
‚ÄĘ
Prematurity.
‚ÄĘ
IUGR
(causes chronic bowel ischaemia).
‚ÄĘ
Hypoxia.
‚ÄĘ
Polycythaemia.
‚ÄĘ
Exchange
transfusion.
‚ÄĘ
Hyperosmolar
milk feeds.
Presentation
Most common in the second week
after birth.
Early
‚ÄĘ
Non-specific
illness.
‚ÄĘ
Vomiting/bilious
aspirate from gastric tube.
‚ÄĘ
Poor
feed toleration (increasing gastric aspirates).
‚ÄĘ
Abdominal
distension.
Late
‚ÄĘ
Additional
abdominal tenderness.
‚ÄĘ
Blood,
mucus, or tissue in stools.
‚ÄĘ
Bowel
perforation.
‚ÄĘ
Shock.
‚ÄĘ
DIC;
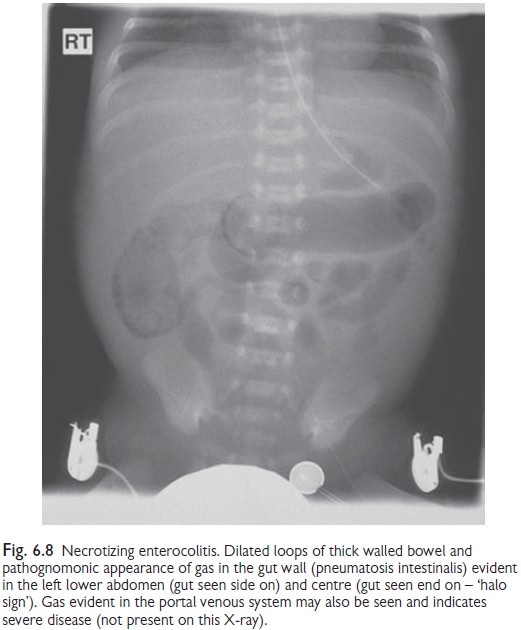
multi-organ failure. AXR shows intestinal distension (see Fig. 6.8).
‚ÄĘ
Pneumatosis
intestinalis.
‚ÄĘ
Hepatic
portal venous gas.
‚ÄĘ
Signs
of intestinal perforation, e.g. free peritoneal gas or gas outlining of falciform
ligament (‚Äėfootball‚Äô sign).
Management
‚ÄĘ
Prophylaxis: antenatal steroids and breast milk
are protective. Emerging evidence for
prevention by administration of probiotic bacteria.
‚ÄĘ
Investigations: FBC; U&E; creatinine;
coagulation screen; albumin; blood gas;
blood culture; AXR; Group and cross match.
‚ÄĘ
Stop
milk feeds for 10‚Äď14 days. Insert gastric tube on free drainage.
‚ÄĘ
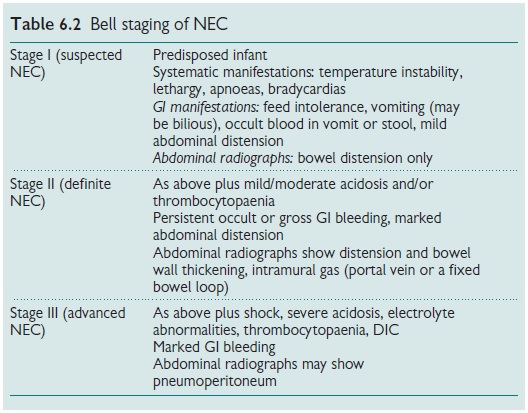
‚ÄėBell
staging’ (see Table 6.2) may be useful in grading severity.
‚ÄĘ
IV
antibiotics for 10‚Äď14 days, e.g. benzylpenicillin, gentamicin, and
metronidazole.
‚ÄĘ
Systemic support: e.g. assisted ventilation, correct
BP and DIC, parenteral nutrition
(PN).
‚ÄĘ
Surgical opinion: indications for surgery are GI
perforation, deterioration despite
above medical treatment (necrotic bowel likely), GI obstruction secondary to
stricture formation (late). If localized disease, surgical resection of
involved bowel with primary repair.
If more extensive, two stage
repair with bowel resection(s) and enterostomy, followed later by intestinal
re-anastomosis.
Prognosis
Overall mortality is 722%.
Increased mortality is associated with:
‚ÄĘ
VLBW.
‚ÄĘ
Extensive
intestine involvement.
‚ÄĘ
Multi-organ
failure.
‚ÄĘ
Intrahepatic
portal gas.
Extensive bowel resection may result in short bowel syndrome. Excellent prognosis is seen in those who respond to medical treatment, but subse-quent stricture may develop.
Related Topics