Chapter: Paediatrics: Neonatology
Paediatrics: Hypoglycaemia
Hypoglycaemia
·
Measurement
of blood glucose using glucose reagent strips is unreliable. Use blood glucose
analyser or laboratory measurement.
·
In
newborn period defined as <2.6mmol/L.
·
Blood
glucose drops naturally in first few hours after birth before
normalising—newborns have increased ability to utilize ketones/lactate for
energy.
·
All
infants should be encouraged to feed in first hour if well enough.
·
At
risk groups for hypoglycaemia include; infant of diabetic mother; <2500g or
<3rd centile for weight; <37/40 gestation; maternal beta-blockers; birth
asphyxia.
·
Check
blood glucose in all infants who are unwell/lethargic/jittery.
Causes
·
Reduced glucose stores: preterm, IUGR, LBW, inborn errors
of metabolism (IEM) (e.g.
galactosaemia).
·
Increased glucose consumption: sepsis, hypothermia, perinatal
hypoxia, polycthaemia, haemolytic
disease, seizures.
·
Hyperinsulinism: maternal diabetes mellitus, BWS,
pancreatic islet cell hyperplasia,
transient.
·
Miscellaneous: maternal Ăź blockers, tissued or
malfunctioning IV infusion.
·
Other rare causes: foetal alcohol syndrome, pituitary
insufficiency, adrenal insufficiency.
Presentation
Commonly asymptomatic.
Jitteriness, apnoea, poor feeding, drowsiness, seizures, cerebral irritability,
hypotonia, macrosomia (if hyperinsulinism).
Investigation
Blood glucose should be measured
in first hour in all high risk infants. Apart from regular blood glucose
measurements, further investigation is not usually required if cause evident
(e.g. IDM).
Suspicious patterns of
hypoglycaemia meriting investigation include;
·
Recurrent
hypoglycaemia in term infant despite functioning intravenous infusion (IVI) of
glucose 10%.
·
Severe
(<1mmol/L) and/or recurrent (>1) hypoglycaemia.
·
Symptomatic
hypoglycaemia.
·
High
glucose requirement (>8mg/kg/min).
·
Hypoglycaemia
and prolonged jaundice (panhypotpituitarism) or sodium abnormalities (adrenal
problems).
Hypoglycaemia with genital or
midline abnormalities.
First line tests (taken when
hypoglycaemic):
·Blood for glucose, insulin, growth
hormone, cortisol, β-hydroxybuyrate, free fatty acids, amino acids (consider
C-peptide, lactate, and ammonia).
·Urine for urinalysis (ketones),
amino and organic acids.
·Further investigations as guided
by results/clinical biochemist.
Prevention
of hypoglycaemia in at-risk infants.
·Adequate feed soon after birth
(<1hr) and then at least 3-hourly.
·Monitor blood glucose levels
(pre-feed), keep warm, support feeding.
Prognosis
Profound/prolonged hypoglycaemia
can cause neurological damage— exact level/duration after which this may occur
is unclear.
Treatment of hypoglycaemia
Symptomatic or severe hypoglycaemia
(glucose<1.0mmol/L)
·
IV
bolus 3–5mL/kg of glucose 10%
·
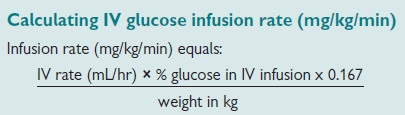
Follow
with 10% glucose infusion IV (4–6mg/kg/min)
Asymptomatic
(glucose <2.0mmol/L or
2.0–2.6mmol/L on 2 occasions)
·
Enterally
fed infants:
· inspect feed chart
(frequency/volume, etc.)
· if reluctant to feed—consider NGT
· if not tolerating milk—consider IV
· give early milk feed (consider
larger volume)
· monitor with pre-feed blood
glucose levels
·
Infants
on IV fluids:
· check IV line is working
· if glucose <1.0mmol/L—give
bolus then increase infusion rate/ concentration
· if glucose >1.0mmol/L—increase
infusion rate/concentration
Resistant hypoglycaemia
(glucose
requirement >8mg/kg/min)
·
Seek
specialist advice, as hyperinsulinism likely
·
Increase
background glucose infusion (central IV access needed)
·
Glucagon
0.5mg IM can be given in emergency—rebound increased insulin secretion will
occur
·
Treatment
options include:
diazoxide (given with
chlorthiazide to counteract fluid retention)
somatostatin (octreotide)
nifedipine
surgery (subtotal pancreatectomy)
·
Enteral
feeding promotes normality. Aim to wean off IV as soon as able
·
High
concentrations of glucose (>12.5%) require central IV access
·
Monitor
plasma sodium if on IV fluids
Related Topics