Chapter: Paediatrics: Neonatology
Paediatrics: High frequency oscillatory ventilation
High frequency oscillatory ventilation
A continuous positive distending
pressure (mean airway pressure) is ap-plied and, around this pressure amplitude
(or ∆p) is oscillated by a dia-phragm or an interrupter device in the
ventilator circuit. High frequency oscillatory ventilation (HFOV) has an
efficacy equivalent to IPPV in the primary treatment of RDS. It may be
indicated for:
· Rescue treatment when IPPV has
failed.
•
Pulmonary
air leaks.
•
Meconium
aspiration syndrome.
•
PPHN.
•
Pulmonar
y hypoplasia.
•
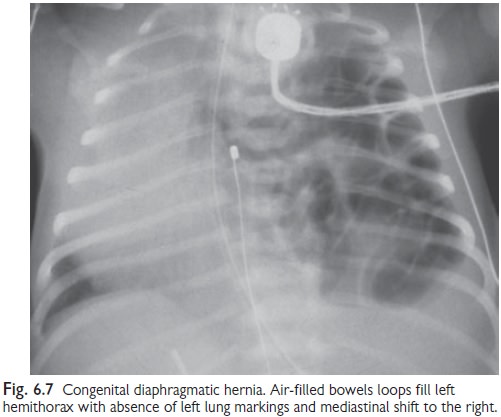
Congenital
diaphragmatic hernia (see Fig. 6.7).
Ventilation parameters
•
Mean
airway pressure (Paw).
•
FiO2.
•
Airway
pressure difference generated around Paw (amplitude or ∆p).
•
Oscillation
frequency per second.
•
Circuit
gas flow.
Oxygenation (PaO2) is
dependent on both Paw and FiO2. As Paw ‘rise’,
PaO2 will improve as functional residual capacity (FRC) ‘rise’. At
some point, how-ever, further Paw ‘rise’ will ‘fall’ PaO2
because of over distension.
CO2 removal (PaCO2)
is dependent on alveolar ventilation and, so, on both the frequency and
amplitude. Unlike IPPV, ventilator constraints make tidal volume inversely
proportional to the frequency. It is normal for generated tidal volumes to be
less than that physiologically required, yet adequate ventilation occurs—this
apparent paradox is explained by com-plicated air flow physics of HFOV that
augment CO2 diffusion. Once the frequency is set, CO2
removal is increased by ‘rise’amplitude and vice versa.
Commencing ventilation
If ventilating for the first time,
appropriate initial settings at term are:
• Paw 8cmH2O.
• Amplitude 20cmH2O.
• Frequency 10Hz.
• FiO2 0.5, i.e. 50%
inspired O2 concentration.
If transferring from IPPV:
• Set initial HFOV Paw
2cmH2O higher then Paw used in IPPV.
•
Start
on the same FiO2, and set frequency at 10Hz.
Monitoring ventilation
•
Once ventilated,
observe the infant’s chest expansion and oscillation, and alter settings as
required.
•
Perform
a CXR after 1hr to assess chest expansion: 8 posterior ribs visible above the
diaphragm is appropriate until the baby is stable.
Monitoring ventilation is
otherwise as for IPPV. Be aware that rapid elimination of CO2 can
occur leading to over-ventilation. Anticipate and monitor blood
gas/transcutaneous readings closely.
•
If PaO2 is too low:
‘rise’either the FiO2 or mean airway pressure (MAP) by 1–2cmH2O every 30–60min
(avoid chest overexpansion), and vice versa.
•
If CO2 is too high: ‘rise’amplitude by 2cmH2O
increments and vice versa.
•
Optimal
CO2 elimination occurs at 10Hz, and, hence, the frequency does not
usually need to be changed.
Weaning ventilation
As clinical status improves:
‘fall’ FiO2 to 0.5 and then ‘fall’ Paw by 2cmH2O
steps until 6–7cmH2O is tolerated. Also progressively ‘fall’ amplitude
to the mini-mum required to maintain normal CO2.
Some babies will tolerate weaning
to what is essentially CPAP, whilst others, below a certain Paw, do
better if changed to slow rate IPPV.
Related Topics