Chapter: Paediatrics: Neonatology
Paediatrics: Acute respiratory diseases
Acute respiratory diseases
All of the diseases presented
below have signs of respiratory distress. Cerebral hypoxia, congenital heart
disease, and metabolic aci-dosis can induce respiratory distress (suspect if
CXR is normal).
Transient tachypnoea of the newborn (TTN)
ŌĆó
Caused
by delayed clearance/absorption of lung fluid after birth.
ŌĆó
Presents
within 4hr after birth. Common after elective CS. CXR: shows streaky perihilar
changes and fluid in lung horizontal fissures.
ŌĆó
Treatment:
supplemental O2. Consider nasal CPAP and antibiotics.
ŌĆó
Spontaneously
resolves within 24hr.
Congenital pneumonia
ŌĆó
Caused
by aspiration of infected amniotic fluid.
ŌĆó
Associated
with prolonged rupture of membranes (PROM), chorioamnionitis, foetal hypoxia.
ŌĆó
Usually
group B streptococci, Escherichia coli,
other Gram ŌĆōve bacteria, listeria, chlamydia.
ŌĆó
Presents
in first 24hr. CXR: patchy shadowing and consolidation.
ŌĆó
Respiratory support: antibiotics (benzylpenicillin, or
ampicillin if listeria, and
gentamicin) after septic screen; chest physiotherapy.
ŌĆó
Prognosis: depends on severity and associated
sepsis or persistent pulmonary
hypertension of newborn (PPHN).
Meconium aspiration syndrome (MAS) (1ŌĆō5/1000 live births)
ŌĆó
5% of
term infants with meconium-stained liquor develop MAS.
ŌĆó
Hypoxia
results in gasping and meconium passage in
utero, a combination that leads to aspiration. Meconium aspiration inhibits
surfactant, obstructs the respiratory tract, and induces pneumonitis.
ŌĆó
Presents
with respiratory distress soon after birth. Associated with pulmonary air leaks
and PPHN. CXR: generalized lung over inflation with patchy
collapse/consolidation +/ŌĆō air leaks.
ŌĆó
Prevention: if liquor is meconium-stained,
delivery should be expedited to
prevent further hypoxia and gasping. If baby is apnoeic at birth, visualize the
larynx and suck out any meconium from larynx/trachea. Tracheal suction is not
recommended for vigorous infants.
ŌĆó
Treatment: supplemental O2;
intermittent positive pressure ventilation
(IPPV) or high frequency oscillatory ventilation (HFOV) if ventilation
required; surfactant; antibiotics (since listeria can cause antenatal meconium
passage); treat any PPHN; consider ECMO if severe.
ŌĆó
Prognosis: mortality <5%. Survivors do
well, but there is ŌĆśriseŌĆÖrisk of asthma and, if extracorporeal membrane
oxygenation (ECMO) is needed, neurological sequelae.
Pulmonary air leaks
Commonly secondary to other
respiratory disease (e.g. RDS, MAS) or to assisted ventilation.
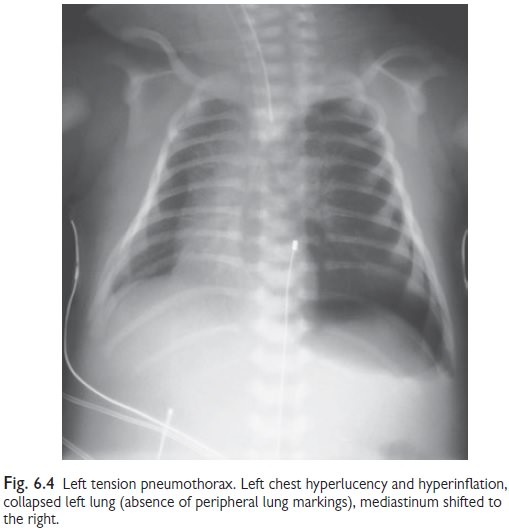
Pneumothorax
Spontaneous pneumothorax occurs in
72% term infants. Incidence is increased in prematurity and respiratory
disease.
ŌĆó
Features: majority are small, asymptomatic,
and resolve spontaneously. If large,
present with respiratory distress. Tension pneumothorax is life-threatening
(signs: respiratory distress, cyanosis, mediastinal shift away from affected
side, ŌĆśfallŌĆÖ chest movement and air entry on affected side, transillumination
lights up affected side).
ŌĆó
CXR: shows ipsilateral translucency,
lack of peripheral lung markings, collapsed
lung (see Fig. 6.4).
ŌĆó
Treatment: none if asymptomatic. Give O2 as required. If symptoms are severe or worsening, insert chest
drain. In emergency, perform needle aspiration before chest drain.
ŌĆó
Prognosis: excellent in term infants.
Mortality is doubled in infants with RDS.
Also ŌĆśriseŌĆÖrisk of periventricular haemorrhage in preterms.
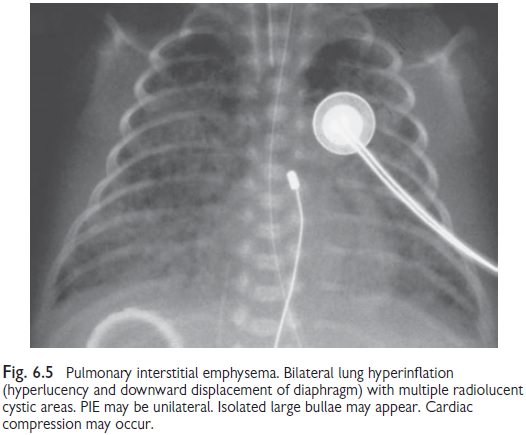
Pulmonary interstitial emphysema (PIE)
Air leak into lung parenchyma
results in small airway and alveolar col-lapse. Follows high IPPV, particularly
in preterm infants with severe RDS or MAS.
ŌĆó Signs:
respiratory distress; chest
hyperexpansion; poor air entry; coarse inspiratory
crackles.
ŌĆó CXR:
hyperinflation; ŌĆśhoneycombŌĆÖ
pattern of cystic lucencies/bullae,
generalized or local (see Fig. 6.5).
ŌĆó Treatment:
high FiO2, low PIP, low
PEEP, fast rate IPPV; HFOV may be
ŌĆó
superior.
Unilateral PIE: nurse infant with affected side down. In refractory cases
consider selective intubation to ventilate the healthier lung.
ŌĆó Prognosis:
mortality 25ŌĆō50%. There is an
increased risk of bronchopulmonary
dysplasia.
Pneumomediastinum
Often preceded by asymptomatic
pneumothorax/PIE.
ŌĆó
CXR: translucency around the heart
extending superiorly; thymus lifted and
splayed from below (ŌĆśsailŌĆÖ sign).
ŌĆó
Treatment: usually no treatment is required.
Pneumopericardium
Usually occurs with other air
leaks associated with IPPV and can
lead to cardiac tamponade (with quiet heart sounds, hypo-tension, bradycardia,
cyanosis).
ŌĆó
CXR: translucency around the borders of
a small heart.
ŌĆó
Treatment: urgent needle drainage inserted
under the xiphisternum.
ŌĆó
Prognosis: high mortality if symptomatic.
Pneumoperitoneum
Air can occasionally track into
the peritoneum from a pulmonary air
leak. AXR confirms the diagnosis. Severe abdominal disten-tion could impair
ventilation. Drain if symptomatic.
Massive pulmonary haemorrhage (1/1000 live births)
Usually due to haemorrhagic
pulmonary oedema in VLBW infants. Small bleeds are associated with tracheal
trauma from ETT or suction. It is associated with: PDA, heart failure, PIE,
hydrops foetalis, perinatal hypoxia, sepsis, coagulopathy, fluid overload,
surfactant therapy
Signs
ŌĆó
Rapid
systemic collapse.
ŌĆó
Profuse
bloodstained fluid welling up from upper airway.
ŌĆó
Respiratory
crackles on auscultation.
ŌĆó
CXR. Virtual
ŌĆśwhite outŌĆÖ. Consider echocardiography to detect PDA.
Treatment
ŌĆó
rise O2
and ventilatory pressures.
ŌĆó
Frequent
endotracheal suction.
ŌĆó
Correct
hypovolaemia and coagulopathy.
ŌĆó
Consider
blood transfusion.
ŌĆó
Consider
surfactant.
ŌĆó
Treat
known associations.
Milk aspiration
Term infants can accidentally
aspirate a feed. The usual causes are:
ŌĆó
Swallowing
incoordination, e.g. preterm, neurological disease.
ŌĆó
Upper
airway or oesophageal disorders, e.g. tracheo-oesophageal fistula,
gastro-oesophageal reflux.
Presentation
Sudden choking or respiratory
distress during or after a feed, often with excessive milk in the mouth, or
aspiration pneumonia.
CXR:
normal or patchy
collapse/consolidation in the upper lobes.
Treatment
If well, observe only. If unwell, respiratory
support and broad spectrum
antibiotics are needed. Investigate cause and use gastric or naso-jejunal tube
feeding. Period of IV fluids or feeding may be necessary.
Apnoea
Apnoea can result from any severe
illness.
Management
ŌĆó
Support
respiration.
ŌĆó
Investigate
and correct primary cause.
Apnoea of prematurity
ŌĆó
Common
below 34wks gestation (incidence ŌĆśriseŌĆÖas gestation d).
ŌĆó
Between
episodes the infant is well.
ŌĆó
Consider
and exclude other diagnoses.
Treatment
Tactile stimulation, blood transfusion,
continuous tube gastric feeds,
caffeine or theophylline, nasal CPAP, or IPPV.
Prognosis
Short-lived apnoeas appear to
cause no harm and should resolve by
34wks gestation.
Related Topics