Chapter: Paediatrics: Neonatology
Paediatrics: Bronchopulmonary dysplasia
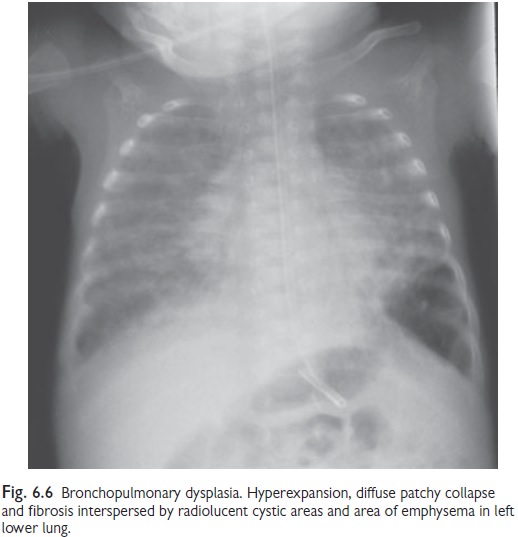
Bronchopulmonary dysplasia
Bronchopulmonary dysplasia (BPD)
is a form of chronic lung disease that affects infants who have been born
preterm. Over the last decade advances in neonatal care, including the
increasing use of antenatal steroids, and early surfactant therapy, have
modified a change in the underlying pathology in many cases. ŌĆśOldŌĆÖ BPD was
described as a disease of scarring, and repair. This condition was associated
with long periods of mechanical ventilation, often with high PIP, and high FiO2.
ŌĆśNewŌĆÖ BPD is a condition of impaired alveolar development, with less
destruction and scarring. Mechanical, oxidative and inflammatory factors all contrib-ute
to lung injury. The radiographic appearances of more recent cases are less
dramatic (see Fig. 6.6), however, the impairment in lung function continues
through childhood, and is associated with a number of other impairments.
Definition
The definition of BPD has evolved
with time. The most commonly used definition is ŌĆśOxygen requirement at 36/40
corrected gestational age (CGA)ŌĆÖ. This definition does not have any grading of
severity, and encom-passes a wide spectrum of disease.
NICHD/NHLBI Definitions (2001)
ŌĆó
Mild: need for supplemental O2 at age 28 days, but not at 36/40 CGA
ŌĆó
Moderate: need for supplemental O2 <30% at age 28 days and at 36/40 CGA
ŌĆó
Severe: mechanical ventilation or
requiring >30% O2 at 36/40 CGA
ŌĆśWalshŌĆÖ test (2003)
ŌĆó
Test
at 36┬▒1/40 CGA. Aim to maintain SpO2 > 88%
ŌĆó
BPD if
need 30% O2 to maintain SpO2
>88% (or ventilated)
ŌĆó
If
<30% O2, then FiO2 is gradually decreased
to air. BPD is defined as inability to maintain SpO2 >88% for 1hr
Incidence and risk-factors
Incidence is dependent on
definition used. Wide variations between cen-tres with a range of 4ŌĆō58% (mean
23%) of at-risk babies. BPD more likely with:
┬Ę Gestational immaturity.
ŌĆó Low birth weight.
ŌĆó Males.
ŌĆó Caucasian heritage.
ŌĆó IUGR.
ŌĆó Family history of asthma.
ŌĆó
History
of chorioamnionitis.
Prevention of BPD
No evidence of effect
ŌĆó
Surfactant
and ANC steroids (effect may be off-set by increased survival?)
ŌĆó
Closure
of PDA
ŌĆó
Diuretics
ŌĆó
Inhaled
steroids
ŌĆó
Inhaled
nitric oxide
ŌĆó
HFOV
compared to conventional ventilation
ŌĆó
Treating
Ureaplasma urealyticum (more research
needed)
May be of benefit in certain infants
ŌĆó
Systemic
corticosteroids (clinical trials needed as increased risk of CP)
ŌĆó
nCPAP
vs. intubation(need for surfactant, risk of pneumothorax)
Evidence of effect
ŌĆó
Caffeine
citrate for apnoea of prematurity in infants <1250g
ŌĆó
Vitamin
A supplementation for infants <1000g
Treatment of established BPD
No specific treatment has been
demonstrated to show an improve-ment in outcome of BPD. Oxygen is the most
commonly used therapeutic agent, although the ŌĆścorrectŌĆÖ dose and what SpO2
is acceptable has not been established. A number of large trials are ongoing
and their results are awaited (Ref: NeOPrOM Collaboration).
Other treatments include;
diuretics, corticosteroids, sildenafil, optimiz-ing nutrition.
Immunization for at-risk infants
with monoclonal respiratory syncytial virus (RSV) antibody has recently been
recommended by the UK depart-ment of health. This involves monthly injections
during the RSV season.
Outcome
Increased survival of preterm
infants has led to an increase in the number surviving with BPD. Mortality has
improved (previously 10ŌĆō20% would die from cor-pulmonale or respiratory
infection). Other problems include:
ŌĆó
Increased
risk of CP.
ŌĆó
Poorer
cognitive functioning and academic performance.
ŌĆó
High
risk of re-hospitalization with respiratory illness.
ŌĆó
Poorer
lung function.
Respiratory problems seem to
lessen as children get older, perhaps reflecting the lungŌĆÖs continued growth
and development.
Related Topics