Chapter: Paediatrics: Neonatology
Paediatrics: Hypoxic‚Äďischaemic encephalopathy
Hypoxic‚Äďischaemic encephalopathy
Clinical syndrome of brain injury
secondary to a hypoxic-ischaemic insult. In developed countries the incidence
is 72‚Äď5/1000 live births (moderate to severe incidence is 1‚Äď2/1000 live
births).
Causes
·
‚Äėfall‚Äô
Umbilical blood flow, e.g. cord prolapse.
·
‚Äėfall‚Äô
Placental gas exchange, e.g. placental abruption.
·
‚Äėfall‚Äô
Maternal placental perfusion.
·
Maternal
hypoxia from whatever cause.
·
Inadequate
postnatal cardiopulmonary circulation.
Presentation
Varies depending on severity of
cerebral hypoxia. An infant may have a range of symptoms and signs affecting:
level of consciousness, muscle tone, posture, tendon reflexes, suck, heart rate
and central nervous system ho-meostasis.1
Before
concluding that an infant may have
HIE secondary to an intra-partum hypoxic-ischaemic
event, assess for evidence of an
intrapartum problem (e.g. CTG abnormality, sentinel event such as abruption
or cord prolapse). There should be respiratory depression at birth and a need
for resuscitation, including IPPV (Apgar score at 5min < 5). There should be
moderate to severe acidosis soon after birth (pH<7.0, base excess worse than
‚Äď12). The baby should develop encephalopathy within 24hr of birth. Other causes
of encephalopathy should be excluded.
Management
·
Resuscitate
at birth; insert IV ¬Ī arterial lines. Avoid hyperthermia.
·
Assess
eligibility for therapeutic hypothermia (TH).
·
Start
cerebral function analysis monitoring (CFAM).
·
Assess
for features of dysmorphism and birth trauma.
·
Assess
neurological features.
·
Exclude
other causes of encephalopathy, e.g. meningitis, metabolic disturbances,
maternal drugs, CNS malformation, and haemorrhage.
·
Expect
and manage associated multi-organ failure, e.g. cardiac or renal.
·
Monitor
and maintain homeostasis, e.g. U&E, Ca2+, Mg2+ blood
glucose, Hb, blood gases, coagulation. Support BP.
·
Mild
fluid restriction initially (e.g. 40mL/kg/day 10% dextrose) as there may be
oliguria. Omit milk feeds for 1‚Äď2 days if HIE severe and then feed slowly.
·
Treat
seizures.
Therapeutic hypothermia
This is now the standard of care
for term infants with moderate/severe hy-poxic ischaemic encephalopathy.2
Cooling is achieved using a temperature controlled mattress or wrap, and
eligible infants have their temperature lowered to 33‚Äď34¬įC within 6hr of
insult. Hypothermia is maintained for 72hr before gradual re-warming.
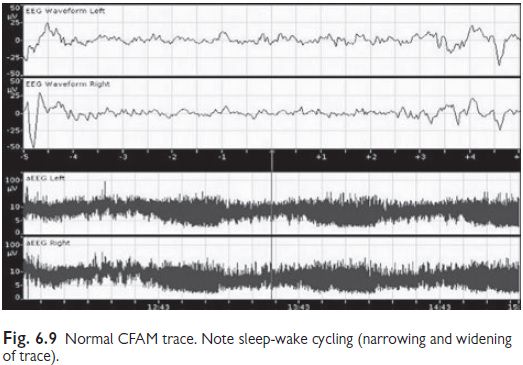
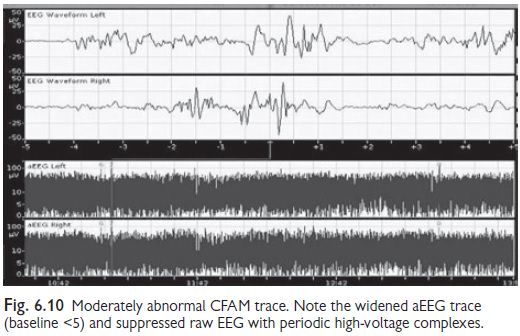
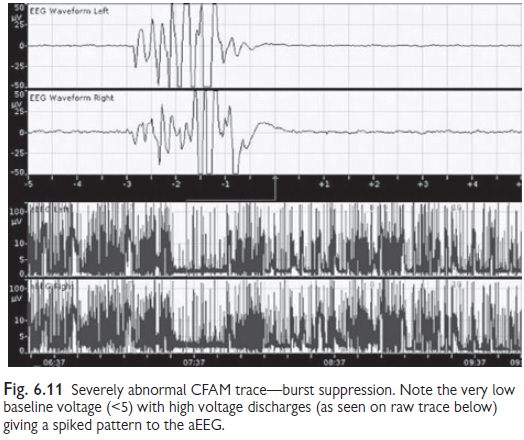
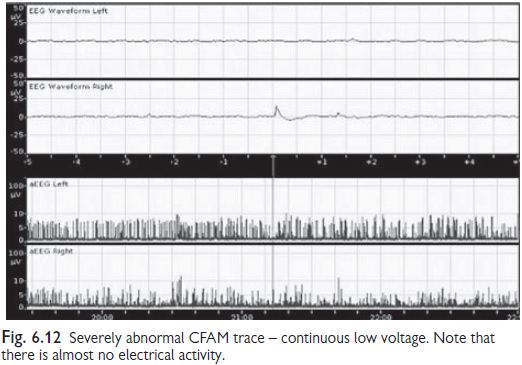
Cerebral function analysis monitoring (CFAM)
Single or 2 channel machines
available (2 channel = left and right hemi-spheres). Displays ‚Äėraw‚Äô EEG and a
compressed ‚Äėamplitude integrated‚Äô re-cording. Pattern of a EEG is used for
classification of background activity (see Figs 6.9‚Äď6.12). Normal CFAM (aEEG)
recording (term infants):
‚ÄĘ
Lower
margin 5¬ĶV (when awake), upper
margin 10¬ĶV.
‚ÄĘ
Evidence
of sleep-wake cycling, no seizures.
Prognosis
Without cooling, risk of later disability or death is: grade I <2%; grade II 24%; grade III 78%. Disabilities are likely to be one or more of the follow-ing: spastic quadriplegia, dyskinetic cerebral palsy, severely reduced IQ, cortical blindness, hearing loss, and epilepsy.
Related Topics